Meeting Cancer Survivors' Psychosocial Health Needs: A Conversation with Dr. Patricia Ganz
, by Elia Ben-Ari
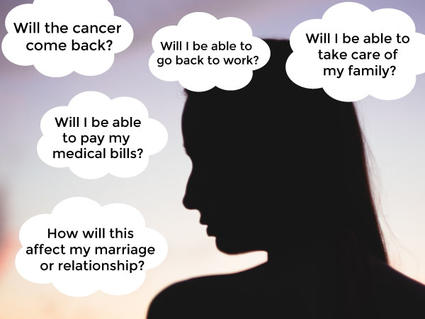
The impact of cancer and its treatment is undeniably stressful. And although many people recover well, about 25% of cancer survivors have persistent problems, including anxiety, depression, and other psychological and social (psychosocial) distress.
In this interview, Patricia Ganz, M.D., of UCLA’s Jonsson Comprehensive Cancer Center, discusses psychosocial distress in cancer survivors and the challenges and opportunities in this area. Dr. Ganz has dedicated much of her career to the study of cancer survivorship; she was on the Institute of Medicine (now the National Academies) committee that published the 2008 report, Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs.
Do you get the impression that most clinicians think about the mental health needs of cancer survivors?
Most clinicians would like to be thinking about these things. However, in the usual short follow-up visits, the appointment is more focused on a patient’s physical symptoms and what needs to be done to follow up on the cancer. So, often the topic of a person’s mental health needs does not come up unless the patient is very anxious or looks depressed. This is especially true for people who have had more intense or complex cancer treatment, where their physical symptoms and the need for follow-up tend to drive the conversation.
However, patients want to know how they can manage their health after cancer—including their mental health. Often the emotional impact of the cancer diagnosis and treatment does not crop up until 6 months or a year after treatment ends. From the outside, a patient may appear to have fully recovered. But in fact, they are suffering inside.
How can clinicians who see cancer survivors address their patients’ mental health concerns?
If the physician or member of the health care team said something like, “We know that recovering from this both physically and emotionally will be difficult. Please let us know if you have had an increase in physical or emotional problems since your cancer diagnosis. We’re here for you, we can make referrals, and there are lots of resources that can help you cope with both the physical and emotional aftereffects of cancer.”
If an oncologist has been through treatment with thousands of patients and knows the spectrum of issues that can arise, why not share that with the patient so they know what to expect?
What are the biggest challenges when it comes to mental health care for cancer survivors?
One of the challenges we face is the stigma in our society of asking for anything that is related to mental health care services. In addition, some survivors may come from cultures where looking for help of this type may be unfamiliar. Another challenge is that we tend to have silos of care [due to the specialized nature of modern medicine]. Things would be a lot easier if we could integrate psychosocial support as part of care and not view it as something separate. And having a clinician who is attentive to the whole person—the mind as well as the body—can help.
Over the past 20 years, my colleagues and I have shown how cancer treatment can affect the brain—for example, by causing inflammation. Our stress hormones are in high gear when we’re going through cancer treatment. In addition, we’ve found that adversity during childhood, such as abuse and neglect, can gear up your stress hormones from an early age to respond to any threat, including the cancer experience, in an intensified way.
Most oncologists don’t appreciate that before a person has ever had cancer, there’s possibly been a slate written for how their mind and body respond to stress. And now you’re throwing lots of potentially toxic treatments at them that increase inflammation, which will engage with a person’s preexisting stress responses.
Are there one or two of these challenges or barriers that would be easiest to address?
NCI's Office of Cancer Survivorship (OCS) hosts the OCS Director's Series of webinars. These webinars examine research on the physical, psychological, social, and economic effects of cancer and its treatment. Watch the presentation by Dr. Ganz for an update on the 2008 Institute of Medicine report Cancer Care for the Whole Patient.
There are short questionnaires, such as the PHQ-4, that screen for anxiety and depression, are easy to use in clinic, and could pick up seriously troubled people with just two questions each on anxiety and depression. But unless you can respond to those problems and connect people with tools and services to help them cope, you haven’t done very much for the person. There are many different things, such as tai chi, yoga, and mindfulness meditation that will help with both the physical and mental aftereffects of cancer.
You don’t even have to ask someone directly if they are depressed—you can ask about mood, sadness, and symptoms that may be indicators of depression, such as fatigue, trouble falling asleep, and trouble concentrating. These things are quite common among cancer survivors, and they will affect a person’s well-being or quality of life and how they’re recovering, even if the person does not meet the criteria for being depressed.
If clinicians prefer not to use a written or electronic questionnaire, they can ask questions from it and then find out how to address those problems.
Are there challenges or barriers to providing psychosocial support for survivors that are more difficult to address?
I think there is a fear among clinicians that if you start to look for mental health issues among patients you would be opening a can of worms and that addressing anxiety and depression would take too much time. But in fact, a recent study of people with breast cancer, led by Erin Hahn, Ph.D., M.P.H., at Kaiser Permanente Southern California, found that fewer than 10% of people who were screened for depression in community-based oncology practices met the criteria for needing a special care referral.
Screening tells the patient that you care about this part of their experience. It also says, if you have some problems in the future, we can find someone to help you. And for those who are struggling now, there’s an acknowledgment that this is one of the issues that people may face when they have cancer.
NCI and others have supported a lot of high-quality research in this area, but the type of care that is needed is not getting delivered. Any kind of behavioral or psychosocial health service, such as psychotherapy or mindfulness training, is just not part of general medical care. And these services are not routinely billable by oncologists or community cancer clinics because of the way our health insurance system is set up.
However, I’m hopeful that this may change because many insurance plans are realizing that persistent mental health issues can lead to the consumption of extra resources. For example, Dr. Hahn and her colleagues showed that, in clinics that screened for depressive symptoms and referred patients who needed help to a behavioral health specialist, there was a decrease in oncology visits. This is not entirely surprising because patients who are worried or anxious often come back to see their doctor more frequently.
For adolescents and young adults (ages 15–39), are there specific issues that you feel are a particularly high priority to address?
Screening for psychological distress and providing mental health care must be the number two priority, after treating the cancer. I regularly have young adults referred to me who have gone through arduous treatment, and when I screen them for depression they are off the charts. Sometimes it’s due to other life experiences from before they had the cancer. But other times it’s because their lives have been derailed by having cancer.
Are there specific things that you see as a higher priority to address regarding the psychosocial well-being of cancer survivors?
Some professional organizations have endorsed screening all cancer patients and survivors for psychosocial distress, which is important. But screening alone is not enough. You have to be able to link people to the many evidence-based, highly effective psychosocial services that NCI research has funded. Studying how to implement and disseminate these kinds of services is critical, and that’s where the rubber hits the road.
My passion now is to find the most effective way to get the tools and strategies that we know can work to the people who need them. We also need to figure out how to normalize the provision of psychosocial health services as part of high-quality cancer care. Clinicians need to have a menu of treatment options available, and if one strategy doesn’t work for somebody, or if they don’t like it and don’t want to use it, there’s another strategy to try. But we can’t give up and say it’s too difficult to meet the psychosocial health needs of cancer survivors.