Shorter Course of Radiation Is Effective, Safe for Some with Early-Stage Breast Cancer
, by Elia Ben-Ari
For some people with early-stage breast cancer, a condensed course of radiation therapy is as safe and effective as a longer standard course, new clinical trial results show.
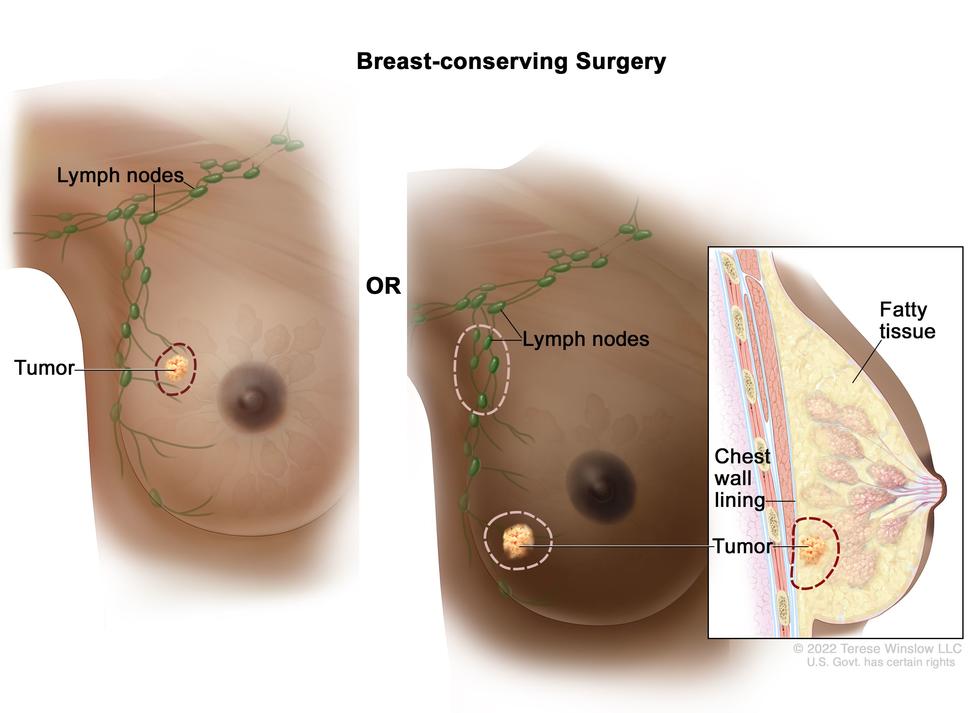
The phase 3 clinical trial enrolled women with early-stage breast cancer who had surgery to remove the tumor (lumpectomy) and had a relatively higher risk of the cancer coming back at the site of the surgery. For these women, the trial found, the time needed for daily radiation therapy could safely be shortened from about 4–6 weeks to 3 weeks.
This shorter course of treatment makes radiation therapy less burdensome for patients, experts said.
For people with higher-risk early-stage breast cancer, the recommended treatment may include an extra 4–8 days of radiation to the area of the breast where the tumor was. Traditionally, this radiation “boost”—which helps reduce the risk that the cancer will come back (recur) in that breast—has been given after 3–5 weeks of radiation, given every weekday, to the whole breast.
But in the trial, the research team found that giving the boost treatments during a 3-week course of whole-breast radiation was as safe and effective as giving the two treatments one after the other.
“We saw very low rates of recurrence at 5 and 7 years [after lumpectomy], with no differences between” the two treatment approaches, said study leader Frank Vicini, M.D., of GenesisCare in Pontiac, Michigan. Dr. Vicini presented the findings of the NCI-funded trial October 24 at the American Society for Radiation Oncology (ASTRO) annual meeting in San Antonio, Texas.
“Just as critical,” Dr. Vicini said at the meeting, there were no differences between the two approaches in terms of their side effects or on the look and feel of the treated breast. And the overall rate of severe side effects was quite low in both groups.
Getting daily radiation treatments for breast cancer often requires taking time off from work. In addition, patients may have to travel long distances to the treatment center and arrange for transportation, childcare, or elder care.
“If you can have equivalent outcomes with fewer days of radiation treatment, that's really important, as it makes it easier for people to receive the care they need for their breast cancer,” said Kilian Salerno, M.D., of NCI’s Radiation Oncology Branch, who was not involved with the trial. “This shorter course requires less time off work or away from family, less days of travel for treatment, and less associated financial hardship.”
Uncertainty about radiation for people with a higher risk of recurrence
After a diagnosis of early-stage breast cancer, radiation therapy following a lumpectomy is used to reduce the chance that the cancer will come back in the same breast. There are multiple options for breast radiation therapy, including whole-breast radiation and partial-breast radiation, Dr. Salerno said, and the decision of which treatment is most appropriate is made jointly between a patient and their radiation oncologist.
For whole-breast radiation, previous studies have shown that 3 weeks of treatment at slightly higher doses is as safe and effective as conventional whole-breast radiation over 5–6 weeks.
However, when the trial began a decade ago, this shorter, more intensive course of radiation, known as hypofractionated radiation therapy, had not yet been widely adopted in the United States, according to Lori Pierce, M.D., of the University of Michigan. Dr. Pierce, who was not involved with the trial, provided expert comments on the findings at the ASTRO meeting.
One reason for this slow adoption, Dr. Pierce said, “was the uncertainty of whether and how to incorporate a boost” of radiation for people who had a higher risk of recurrence.
Testing a sequential versus concurrent radiation boost
The trial included 2,262 women with early-stage breast cancer who had a lumpectomy and an elevated risk of recurrence in the same breast. Risk factors for recurrence included higher tumor grade, being younger than 50 years old, having cancer in lymph nodes in the armpit region, and having a hormone receptor–negative breast cancer.
In addition, Dr. Vicini said, 60% of participants had received chemotherapy prior to radiation, which is another sign that a person’s risk of recurrence may be higher.
The trial, known as NRG Oncology/RTOG 1005, was run by the NCI-funded NRG Oncology clinical trials group.
Half of the participants were randomly assigned to receive conventional whole-breast radiation given 5 days a week for 3–5 weeks, followed by a boost given over 6–7 days (sequential boost). The other half received the boost doses during 3 weeks of hypofractionated whole-breast radiation given 5 days a week (called concurrent boost). Participants were followed for a median of 7.4 years.
Cancer recurrence rates after 5 and 7 years were very similar in women who received a sequential boost and in those who received a concurrent boost. The percentage of people who had severe side effects was also about the same. Side effects of radiation therapy may include fatigue, hair loss, and effects on nearby organs, including the heart.
| Recurrence/side effect rate | Sequential Boost | Concurrent Boost |
|---|---|---|
| 5-year recurrence rate | 2.0% | 1.9% |
| 7-year recurrence rate | 2.2% | 2.6% |
| Rate of severe side effects | 3.3% | 3.5% |
Radiation therapy can also cause changes to the look and feel of the treated breast. Importantly, Dr. Pierce said, these effects, as judged by both patients themselves and their physicians, also did not differ between the sequential and concurrent boosts.
Shorter radiation course ready for broad use
Because the trial was conducted at large medical centers as well as smaller community cancer centers and required careful quality control of the radiation treatment procedures at each center, “the results show that use of a concurrent boost can be implemented in many clinics,” Dr. Salerno said. “We can move forward [with] delivering the radiation boost concurrently for appropriate patients.”
She also emphasized that not all people with early-stage breast cancer need a radiation boost, and “whether to incorporate one is a discussion for each person with their treatment team.”
Other large, ongoing clinical trials, including one in the UK and one in Germany, are also looking at this question, Dr. Salerno said, “so there will be even more data addressing this [approach].”
Radiation oncologists are continuing to refine the way that radiation therapy is given for breast cancer and other cancers, including studying ways to further shorten treatment times without reducing the overall effectiveness of the treatment, Dr. Salerno said.
“Thanks to [the NRG Oncology/RTOG 1005 trial] … we can continue to individualize the treatments for breast cancer and also maximize convenience for patients,” Dr. Pierce concluded.