Can Chronic Graft-Versus-Host Disease Be Prevented?
, by Sharon Reynolds
For some people with aggressive blood cancers, such as certain types of leukemia, a treatment called an allogeneic stem cell transplant can provide the most wished-for outcome in cancer treatment: a cure.
But sometimes, the procedure results in a long-term, debilitating condition known as graft-versus-host disease (GVHD). GVHD occurs when immune cells from the donor that are given along with the stem cells during transplantation attack healthy tissues in the recipient’s body along with the cancer cells.
A new study reports what may be a way to prevent chronic GVHD after a stem cell transplant: by removing immune cells called naive T cells from the donated cells before they are transplanted. The researchers found that this substantially reduced the risk of chronic GVHD among study participants without any apparent increase in their likelihood of relapse.
“It’s a strategy that seems to hit the sweet spot” between preserving the delivery of beneficial immune cells and preventing chronic GVHD, explained Marie Bleakley, M.D., Ph.D., of the Fred Hutchinson Cancer Research Center, who led the study.
In three small clinical trials, only 7% of 138 patients who received a naive T cell–depleted transplant developed chronic GVHD, compared with more than 40% of a group of similar patients who received a standard transplant at the same cancer center in the past. Of the cases of chronic GVHD that did develop in patients who got the experimental transplant, none were severe.
Results from the trials were published together January 10 in the Journal of Clinical Oncology.
The trials were all nonrandomized phase 2 trials, meaning that all participants received the experimental treatment. Dr. Bleakley and her colleagues are currently performing two randomized studies to confirm these early results.
Randomized studies are needed before changes to the standard transplant regimen could be adopted, explained Steven Pavletic, M.D., of NCI’s Center for Cancer Research. “But if we can do allogeneic transplants without patients suffering from [chronic] GVHD, that’s huge,” he said.
Stem cell transplants: The original cancer immunotherapy
Blood cancers arise from stem cells in bone marrow that produce the body’s blood cells, including the white blood cells needed to fight infections. As part of treatment for some aggressive types of blood cancer, people may receive an allogeneic stem cell transplant.
This procedure destroys the bone marrow, where the stem cells reside, with high doses of chemotherapy and sometimes radiation therapy. Then, the patient gets an infusion of healthy stem cells from a donor, often a family member, matched to minimize the risks of transplant rejection and GVHD.
These stem cells travel to the bone marrow and, over time, provide the patient with all-new blood cells. In addition, the immune cells infused along with the stem cells will hopefully recognize and kill any remaining cancer cells in the body, a phenomenon called the graft-versus-leukemia effect.
“Allogeneic stem cell transplant is a form of cancer immunotherapy,” said Dr. Pavletic. “It’s been around for more than 50 years, but it’s really the precursor of [things like] CAR T-cell therapy that we have today.”
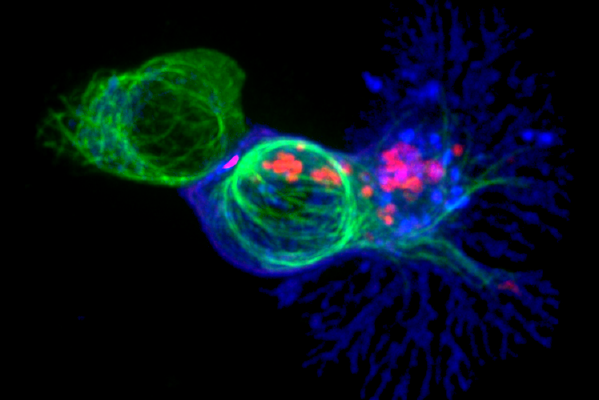
T cells are among the many types of immune cells that can attack cancer cells. But there are several subsets of T cells. Naive T cells have never encountered an antigen—a protein or other molecule that can provoke an immune response. For reasons that are not yet fully understood, they are more likely to react to healthy cells in the transplant recipient.
If immune cells attack and damage those healthy tissues, GVHD can result. GVHD can develop within a few months of the transplant, which is called acute GVHD. The most commonly damaged organs in acute GVHD are the skin, liver, and intestines.
For some people, acute GVHD can resolve with the use of immunosuppressive drugs. GVHD that develops later and has certain distinct characteristics—including specific changes to the skin, mouth, eyes, and joints—is considered chronic GVHD, explained Dr. Bleakley.
“Chronic GVHD is often a really serious condition and can last months to years,” said Dr. Bleakley. “It’s the primary cause of disability and chronic disease in [stem cell] transplant recipients,” she added. In some people, the condition can be fatal.
And if someone develops chronic GVHD, they may need to be on drugs that suppress their immune system for many years.
Immune-suppressing drugs can have side effects and increase the person’s risk of infection. They can also cause problems if a cancer recurs, explained Dr. Bleakley. People generally can’t receive immunotherapies like CAR T cells while on these drugs, but they can’t stop taking them without the risk of their GVHD worsening. “Then we’re in a sort of Catch-22 position,” she said.
Targeted T-cell depletion: Getting rid of naive T cells only
Researchers had previously tried removing all T cells from donated cells before transplantation, a strategy called T cell depletion. But not all T cells are created equal. Without memory T cells, for example, which have prior exposure to and can remember specific pathogens, many people developed severe or fatal infections after their transplants.
The idea to remove only naive T cells emerged almost two decades ago, explained Warren Shlomchik, M.D., director of Hematopoietic Stem Cell Transplant and Cell Therapy at the UPMC Hillman Cancer Center in Pittsburgh, the study’s senior investigator.
At the time, while working at Yale University, Dr. Shlomchik and his colleagues looked at the difference between the contribution of naive and memory T cells to GHVD. “When we realized that memory cells caused less GVHD, we saw the opportunity to translate [that finding] from the bench to the bedside,” he said.
To pull specific types of T cells out of donor grafts, they adapted a laboratory technique for separating cells that uses antibodies joined to microscopic iron beads. The antibodies are engineered to bind to proteins found only on specific types of T cells. The donor blood is then passed by a magnet, which latches on to the iron beads, removing only the unwanted T cells from the graft.
His team quickly saw the potential for the technique to be used in the clinic. In 2005, they joined NCI’s Developmental Therapeutics Program Rapid Access to Intervention Development (RAID) program, which was designed to translate ideas from basic research into testable treatments.
They then partnered with Fred Hutchinson, which has one of the largest stem cell transplant programs in the United States, and brought a biotechnology company partner on board to manufacture a product needed for the selective T cell–depletion method.
Over the next decade, the clinical team at Fred Hutchinson tested the strategy in three early-phase trials. They started out using high doses of chemotherapy and radiation therapy before transplantation—known as the conditioning regimen—which limited participation to younger, healthier people.
Over time, the researchers found that less-intensive conditioning regimens could also be used. This allowed the team to increase the upper age limit for participation from 55 to 60 years old for the third trial.
Between 2009 and 2020, 138 people with acute leukemia received the naive T cell–depleted transplants. All participants also received the standard drugs given immediately after transplantation to prevent GVHD. By the time the results were published, surviving study participants had been followed for a median of 4 years.
Going head-to-head against the standard of care
Almost three-quarters of the participants developed mild acute GVHD, mostly affecting the upper gastrointestinal tract. Participants who developed acute GVHD were less likely to have their cancer return or to die, which Dr. Bleakley attributed to the graft-versus-leukemia effect.
Of the 7% of participants who developed chronic GVHD, in nearly all cases the symptoms were mild and none were severe. By comparison, between 42% and 45% of people who previously received standard stem cell transplants at Fred Hutchinson developed chronic GVHD.
Slightly more than 20% of participants who received the naive T cell–depleted transplants had a relapse of their cancer, similar to what has been seen in historical comparison groups. This, and similar odds of survival compared with people who had received standard transplants, suggests that the graft-versus-leukemia effect was not compromised by removal of the naive T cells, Dr. Bleakley explained.
Two small randomized trials—one in adults and one in children—are now directly comparing rates of chronic GVHD in people randomly assigned to receive one of three types of transplants: naive T cell–depleted transplants, standard transplants, or a type of transplant that has come into wider use recently. Patients receiving this last type will get the chemotherapy drug cyclophosphamide immediately after transplantation, which can suppress T cells likely to attack the recipient’s tissues.
In addition to the goal of lowering rates of chronic GVHD with naive T cell–depleted transplants, “we [also] want high survival rates and low relapse rates,” she continued. “Is what we’ve developed really better than the standard of care? We think so, but we can’t know until we actually do the randomized trials.”
The ongoing trials will also determine whether this method for depleting naive T cells can be replicated at other hospitals. The initial experience in the pediatric trial showing feasibility in replication of the technique have been encouraging, Dr. Bleakley explained.
“We’ve trained half a dozen other centers, and they’re getting really nice results for the naive T cell depletion [so far],” she said.
If the results from the ongoing trials turn out as hoped, the new technique will also need to be tested in older adults, said Dr. Pavletic. All participants in the ongoing randomized trials are aged 60 or younger, but “about 80% of [blood] cancers occur in patients older than 60,” he explained. Currently, stem cell transplants are rarely used in people over age 75, he added.
The Fred Hutchinson team had begun testing a combination of the less-intensive conditioning regimens used for older patients and naive T cell depletion as part of the recently published study, Dr. Bleakley said.
When she and her colleagues first began these trials, she explained, they weren’t sure whether intensive conditioning regimens were a prerequisite for transplants to work—that is, take up residence in the bone marrow and begin making healthy blood cells, known as engraftment.
“But in the last trial, we had half the patients receive a less-intensive conditioning regimen and their engraftment was just fine. So we think we can back off [the intensity even further],” she said.