Obesity May Help Tumors Survive and Grow, Mouse Study Suggests
, by Sharon Reynolds
Obesity alters many processes in the body, from how sugar is used to how the heart functions. It can also change the relationship between cancer cells and nearby immune cells in ways that help tumors survive and grow, according to a new study conducted largely in mice.
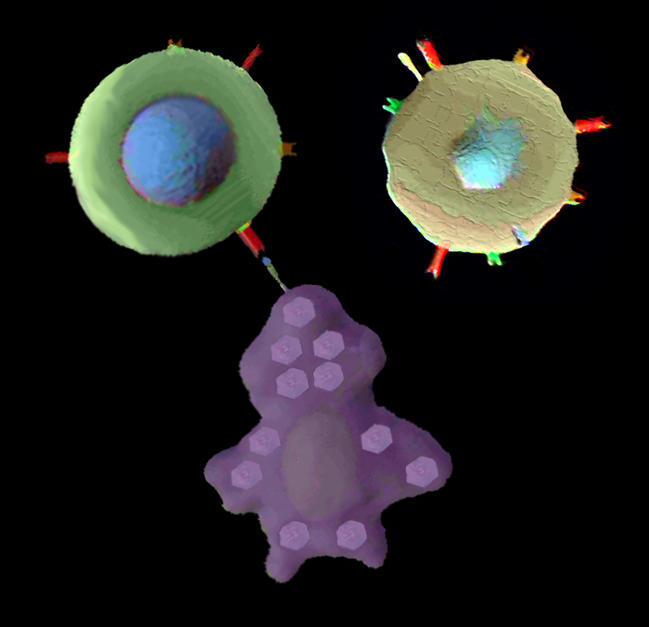
Immune cells called T cells help the body fight off infections, and in some cases can recognize and kill cancer cells. Many immunotherapies for cancer work by boosting the potency of T cells, particularly a subtype called CD8+ T cells, which are the primary cancer cell–killing T cells.
But obesity may render these T cells less powerful. The new research showed that cells within and around tumors in obese mice had drastic alterations in their metabolism (the way they generate and consume energy). These alterations led to CD8+ T cells being largely locked out of the tumor—and unable to function when inside the tumor—while the tumor cells thrived.
A similar phenomenon appeared to be at work in many samples of tumor tissue taken from people with severe obesity, the researchers reported December 23, 2020, in Cell.
“Cancer immunotherapy has really changed the face of cancer care, but it only works in a subset of patients. We need to understand why some people respond and others don’t respond,” said Arlene Sharpe, M.D., Ph.D., of Harvard University, who led the study along with Marcia Haigis, Ph.D., also from Harvard.
“Individuals with cancer are diverse,” Dr. Haigis said. “There's diversity in age, in body mass, in metabolic state and fitness. This study was really our first step into understanding how obesity affects immune cells in the tumor microenvironment.”
While it’s still too early to understand how changes in metabolism within the tumor microenvironment may affect cancer therapies, it highlights a phenomenon that warrants further investigation, she added.
A Metabolic Tug of War
Scientists’ understanding of the role of fat cells in the human body was upended in the 1990s with the discovery of a hormone called leptin, explained Kristine Willis, Ph.D., of NCI’s Division of Cancer Biology, who was not involved with the study. Until then, fat had largely been considered passive storage tissue, holding excess nutrients for the body to use later.
But leptin, produced by fat cells, was found to actively affect appetite and body weight. Since then, Dr. Willis said, “we’ve found that fat secretes all sorts of chemical substances that act as signaling molecules.” Signaling molecules are molecules in a cell that work together to control cell functions or communicate with other cells in the body.
Previous studies have indicated that obesity can directly affect tumor cells, including how some hormones communicate with them. But how obesity impacts the interactions between tumor cells and immune cells is a relatively new area of study.
It’s known that rapidly growing tumor cells consume a high level of nutrients, which could potentially limit the fuel available to other nearby cells. “We wanted to understand if there would be a metabolic tug of war, if you will, between the CD8+ T cell and the tumor cell,” explained Dr. Sharpe.
The research team began by feeding mice a high-fat diet for up to 10 weeks, until the mice gained enough weight to be considered obese. Then they implanted colorectal cancer cells into both the obese mice and normal-weight mice. The cells used for the experiments normally produce tumors in mice that can easily be infiltrated by immune cells.
Tumors in the obese mice grew faster than tumors in normal-weight mice. When the researchers looked at the immune cells in and around the tumors, they found fewer T cells in the tumors of obese mice. The T cells that managed to make it inside the tumors showed signs that they weren’t functioning normally.
However, T cells elsewhere in the body appeared to be normal. When the team repeated some of the experiments with other cancer types, they saw a similar loss of T cell function in some, but not all, cancer models.
Because tumor cells and immune cells use many of the same fuel sources within the body—and within the tumor itself—the researchers analyzed the metabolic behaviors of different cells within the tumor microenvironment in the obese mice.
They found that tumor cells altered their metabolism to vacuum up any surplus fatty acids around them. In contrast, immune cells didn’t make similar changes, so they ended up without the nutrients they needed to do their job.
Although the current study looked at metabolism specifically, obesity could have other effects besides changing the way that tumor cells use nutrients, Dr. Willis explained. For example, fatty acids can also serve as signaling molecules. “So, while fatty acids are a fuel source for the tumor, at the same time, they may [also] be telling an adjacent immune cell something like ‘stop proliferating,’” she said.
Shutting Down Tumor Cell Metabolism
The researchers then wondered: could interfering with tumor cells’ ability to consume fatty acids slow tumor growth? To test the idea, they engineered tumor cells to overproduce a protein called PHD3, which slows a cell’s ability to take up fatty acids.
When injected into obese mice, the tumor cells with extra PHD3 developed into tumors that consumed less fat than tumors that developed from unaltered cells.
In addition, immune cells were much more likely to infiltrate the PHD3-overexpressing tumors and appeared to work normally.
To see if similar changes in T-cell metabolism could be found in the microenvironment of human tumors, the researchers looked at data from patients with colorectal cancer taken from The Cancer Genome Atlas (TCGA). They found that signs of healthy T cells were reduced in tumors from severely obese patients.
And in five out of six cancer types from TCGA that the researchers examined, tumors that were considered “cold” tumors—that is, tumors not recognized by immune cells (and likely do not respond to immunotherapy)—were more likely to have lower expression of PHD3.
While it’s too early to know if a treatment that modulates PHD3 in cancer cells can be used therapeutically, “it would be interesting to identify other targets that affect this push–pull, because ideally, you would want to starve the tumors of the fuels and [at the same time] activate T cells that kill the tumor cells,” said Dr. Haigis.
Scratching the Surface of a Complex Relationship
Many additional factors could play a role in the interactions between T cells and tumor cells, Dr. Willis explained. Everything from the food that people eat to the bacterial makeup, or microbiome, in their gut and other parts of the body may affect these interactions.
“And there are many other immune cell types within the tumor microenvironment” that this study didn’t examine, Dr. Sharpe said.
Additionally, the effects of obesity on that microenvironment are likely to be different between cancer types, and even between people with the same type of cancer, she explained. For example, some studies have suggested that obesity may make immunotherapy for some cancer types—such as kidney cancer—less effective. But other studies have found that people with melanoma may be more, not less, likely to respond to an immune checkpoint inhibitor if they’re obese.
“This [study] is really just scratching the surface of a very important aspect of cancer biology,” Dr. Willis said. It highlights the importance of a systems biology approach to cancer research: not just studying a single element in the body, but examining how all of the elements interact with each other, she said.