Tumor and Stromal Cellular Interactions
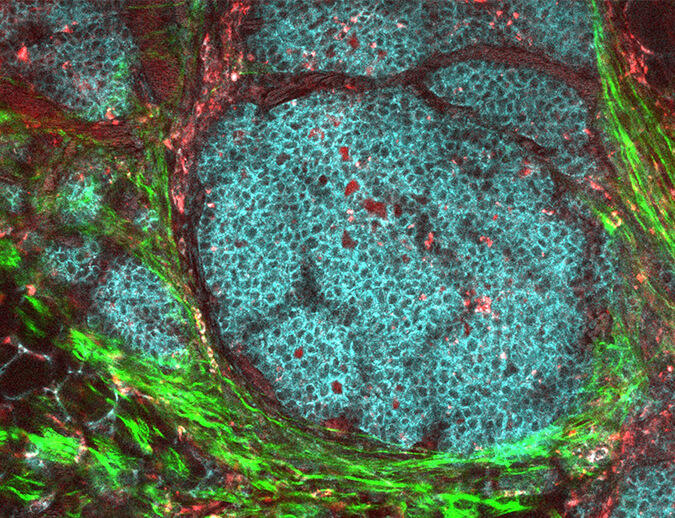
Understanding tumor growth and immune evasion requires characterization of the interactions of
tumor cells with host tissue molecules and the host immune system. Bidirectional interactions between tumor cells and their microenvironment can promote tumor survival and aggressive cell behavior.
Key research areas include:
- Tumor cell-mediated effects on the stromal microenvironment via release of cytokines/growth factors
- Tumor cell and stromal fibroblast-driven inflammation and its influence in the recruitment and function of immune cells in the TME
- Cell-cell, cell-matrix, and exosome-mediated signaling driving tumor cell survival, proliferation, motility and invasion
- Role of physical properties of tumor in communication between tumor and host
- Emergence of tumor organization and progression from molecular and cell-level changes.
The complexities associated with signaling crosstalk pose a significant challenge in the clinic, especially within the context of disease recurrence. Studies dedicated to understanding therapy-associated compensatory pro-survival and pro-growth signaling are expected to help guide future treatments – as will studies on potentially opposing functions of known and emerging targets in the context of either the tumor mass or stroma.
Extracellular Matrix and Tumor Dynamics
The extracellular matrix (ECM), a complex network of proteins, polysaccharides and growth factors, is a major component of the TME. Research in this area focuses on how the ECM becomes disorganized in cancer tissues and promotes cellular transformation.
Key research areas include:
- Cells that alter the ECM during carcinogenesis, including stromal cells and infiltrates
- The biomechanical properties of the ECM including how cells sense external forces, and how the increased stiffness of tumor stroma influences cancer progression
- Mechanisms by which abnormal ECM deregulates stromal cells
- Effects of abnormal cancer ECM on immune cell behaviors related to tumor progression.
- Desmoplasia (the formation of fibrous connective tissue) as a physical barrier to the infiltration of stromal cells (e.g., endothelial, immune, and fibroblast subtypes)
Emerging areas include the role of ECM proteins, matrix remodeling enzymes, and cytokines in driving directional cell migration, and the contribution of the ECM to stem cell maintenance, tumor initiation, progression, and resistance to therapy.
Angiogenesis and Lymphangiogenesis
Research in angiogenesis focuses on tumor-induced vasculature, which provides oxygen and metabolites for tumor growth and progression. Studies on lymphangiogenesis examine the role of tumor-induced lymphatic vessels in tumor cell invasion and migration.
Key research areas include:
- The network of growth factors and receptors that contribute to tumor angiogenesis
- Inducers of neovascularization, including signaling pathways, membrane-derived molecules, secreted factors, and hypoxia
- Molecular strategies that promote vascular normalization to disrupt cancer progression
- Lymphatic vessel invasion and the interplay between a tumor and its lymphatic network
Emerging areas include how altered endothelial cell-pericyte interactions, abnormal blood flow and increased vascular permeability contribute to tumor heterogeneity, therapeutic resistance, and differential immune responses.
Tumor Cell Plasticity
Tumor cells are highly adaptive and known to undergo genetic, epigenetic, and phenotypic changes throughout tumorigenesis. This plasticity contributes to intra-tumoral heterogeneity and is a significant challenge for current cancer therapies. TBMB supports studies aimed at better understanding the pre- and post-therapy induced mechanisms modulating cell plasticity, and the effect of plasticity on tumor heterogeneity, progression, therapy response and resistance.
Key research areas include:
- Role of microenvironment in tumor cell reprogramming, including de-differentiation and trans-differentiation
- Mechanistic characterization of permissive or suppressive tumor microenvironment states in cancer development and progression
- Functional heterogeneity arising from stromal plasticity and various fibroblast and endothelial cell subtypes
Therapy-induced reprogramming of cancer and stromal cells is emerging as an important mechanism of resistance and recurrence. Studies evaluating “reversible” phenotypes and stromal cell states modulated by epigenetic transcription factors in cancer cells may guide the identification of key therapeutic targets.
Cellular and Microenvironmental Aging in Tumors
Age is a well-recognized risk factor for cancer development, and older patients typically develop more aggressive and therapy-resistant tumors. Evidence indicates that aging cells and the aging microenvironment play a direct role in driving tumorigenesis.
Key research areas include:
- Mechanisms of age-related accumulation of senescent cells in tumors and the surrounding stroma
- Effects of senescence-associated phenotypes and/or secretome (e.g., secreted factors) in tumor cell survival, angiogenesis, and therapy resistance
- Metabolic alterations in the aged TME that promote cancer progression and therapeutic resistance
- The effects of senolytics and senomorphics (drugs that target or modulate the activity of senescent cells) on the tumor and TME
Older patients often respond less favorably and with higher toxicity to standard of care, which is emerging as a critically important area of research. Mechanistic studies in this realm help address important questions to ultimately improve cancer treatments during late adulthood and potentially contrast with pediatric tumors that may follow differential tumor-stromal dynamics.
Metabolic Reprogramming of the Tumor Microenvironment
TBMB supports research on how metabolic dysregulation in tumor stroma contributes to and affects tumor progression and resistance to therapy.
Key research areas include:
- Bidirectional alterations in tumor cell/stroma metabolism and its impact on tumor growth and progression
- Tumor cell-mediated metabolic reprogramming of stromal cells and tumor-associated inflammation
- Tumor evolution resulting from stressors (such as systemic therapy, chronic metabolic disorders, localized hypoxia, or nutrient starvation) in the context of the dynamic TME
Emerging areas relevant to this research include the role of metabolic heterogeneity at the cellular level — along with the influence of stromal metabolic gradients — on tumor growth, progression and resistance to therapy, and the role of inter-cellular organelle communication in tumor evolution.
Hormonal Signaling and Tumor Progression
Although abnormal hormonal signaling is associated with certain types of cancers and hormone therapy (which blocks hormonal signaling) is often used in cancer treatments, tumor cells can develop a hormone-resistant, aggressive phenotype. Research on hormonal signaling examines mechanisms that disrupt endocrine signaling pathways in tumor cells and microenvironmental cues that promote tumor progression and resistance.
Key research areas include:
- Biology of hormone-resistant, aggressive tumors
- Mechanisms that change hormone-responsive tumors into invasive, hormone non-responsive tumors
- Identification of novel therapeutic targets of hormone non-responsive tumors
- Biological impact of anti-hormonal therapy on stromal response
Understanding cancer and stromal cell plasticity within the context of naïve tumor progression or in response to therapy are emerging as important areas of research. Elucidation of epigenetic regulators, non-coding RNAs, and genome-wide landscape alterations in mediating tumor and stromal cell phenotype switching and cell state(s) are of interest and informing new translational strategies.
Glycobiology
Research on the glycobiology of tumors explores the role of glycan modifications in malignant progression. Altered glycosylated structures on molecules in tumor cells impact cell-cell and cell-stromal interactions, ligand-receptor affinity, cell signaling, and ultimately cellular functions such as growth, survival and migration processes.
Key research areas include:
- Role of glycans, glycosyltransferases, glycosidases, and lectins in tumorigenesis
- Impact of differential glycosylation on tumor cell-microenvironment interactions
- Development of new, high-throughput technologies and experimental models to investigate glycobiology in the pathogenesis of cancer
- Role of glycosylation in signal amplification and/or attenuation
Emerging areas include the role of glycosylation and other post-translational modifications (phosphorylation, acetylation, ubiquitination, etc.) in protein function and tumorigenesis; and in elucidating the molecular pathways involved in aberrant glycosylation in inter-cellular communication at different stages of tumor development.