Infantile Choriocarcinoma of the Liver
Infantile choriocarcinoma of the liver is a very rare type of cancer that starts in the placenta and spreads to the fetus. The tumor is usually found during the first few months after the baby is born.
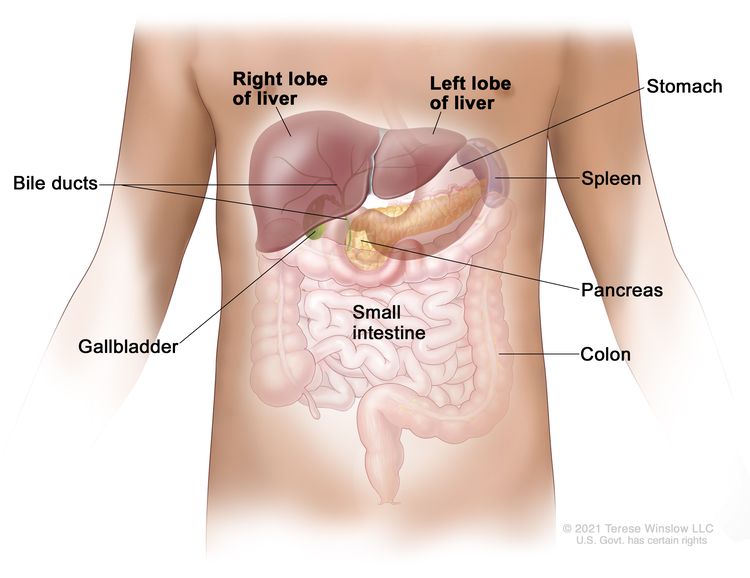
The liver is one of the largest organs in the body. It has two lobes and fills the upper right side of the abdomen inside the rib cage. Three of the many important functions of the liver are:
- to make bile to help digest fats from food
- to store glycogen (sugar), which the body uses for energy
- to filter harmful substances from the blood so they can be passed from the body in stools and urine
The mother of the child may also be diagnosed with choriocarcinoma. For more information on the treatment of choriocarcinoma in the mother, visit Gestational Trophoblastic Disease Treatment.
Symptoms of infantile choriocarcinoma of the liver
Children may not have symptoms of infantile choriocarcinoma of the liver until the tumor has grown bigger. It's important to check with your child's doctor if your child has:
- a lump in the abdomen
- swelling in the abdomen
- hemorrhage
- weakness or increased sleeping
- paleness (loss of normal color from the skin or inside of the nose and mouth)
- shortness of breath
- signs of puberty
- slow growth, poor eating, or is not meeting developmental milestones
These symptoms may be caused by problems other than infantile choriocarcinoma of the liver. The only way to know is to see your child's doctor.
Tests to diagnose infantile choriocarcinoma of the liver
If your child has symptoms that suggest infantile choriocarcinoma of the liver, the doctor will need to find out if these are due to cancer or another problem. The doctor will ask when the symptoms started and how often your child has been having them. They will also ask about your child's personal and family medical history and do a physical exam. Based on these results, the doctor may recommend other tests. If your child is diagnosed with liver cancer, the results of these tests will help you and your child's doctor plan treatment.
The tests used to diagnose infantile choriocarcinoma of the liver may include:
Serum tumor marker test
Serum tumor marker tests measure the amounts of certain substances released into the blood by organs, tissues, or tumor cells in the body. Certain substances are linked to specific types of cancer when found in increased levels in the blood. These are called tumor markers. The blood of children who have liver cancer may have increased amounts of a hormone called beta-human chorionic gonadotropin (beta-hCG) or a protein called alpha-fetoprotein (AFP). Other cancers, benign liver tumors, and certain noncancer conditions, including cirrhosis and hepatitis, can also increase AFP levels.
Complete blood count (CBC)
A CBC checks a sample of blood for:
- the number of red blood cells, white blood cells, and platelets
- the amount of hemoglobin (the protein that carries oxygen) in the red blood cells
- the portion of the blood sample made up of red blood cells
Liver function tests
Liver function tests measure the amounts of certain substances released into the blood by the liver. A higher-than-normal amount of a substance can be a sign of liver damage or cancer.
Blood chemistry studies
Blood chemistry studies measure the amounts of certain substances, such as bilirubin or lactate dehydrogenase (LDH), released into the blood by organs and tissues in the body. An unusual amount of a substance can be a sign of disease.
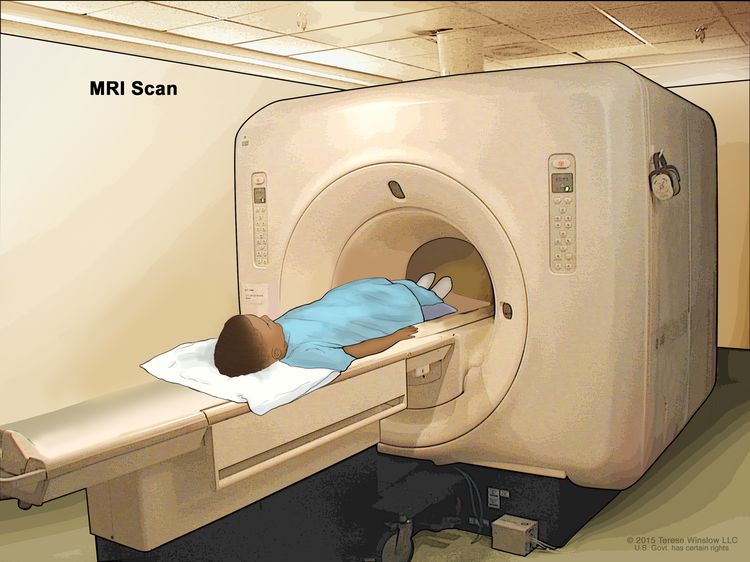
Magnetic resonance imaging (MRI) with gadolinium
MRI uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the liver. A substance called gadolinium is injected into a vein. The gadolinium collects around the cancer cells so they show up brighter in the picture. This procedure is also called nuclear MRI.
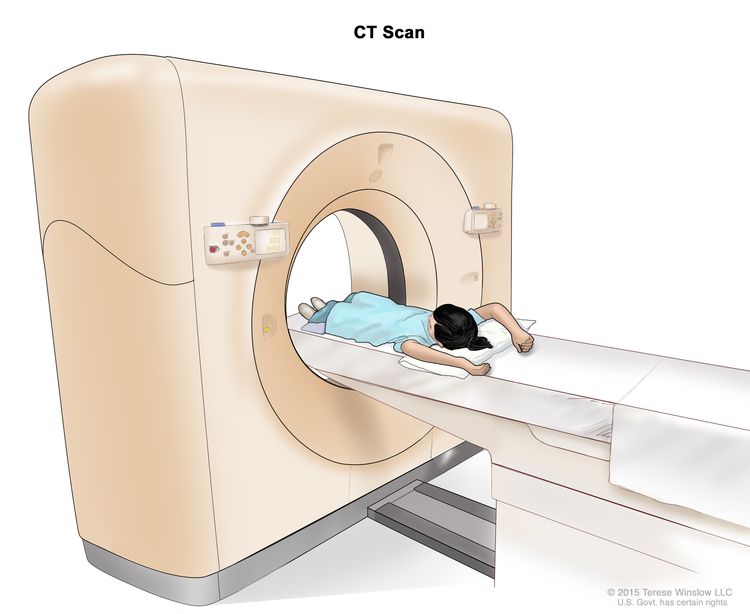
CT scan (CAT scan)
A CT scan uses a computer linked to an x-ray machine to make a series of detailed pictures of areas inside the body, taken from different angles. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography.
A CT scan of the chest and abdomen is usually done to help diagnose childhood liver cancer.
Learn more about Computed Tomography (CT) Scans and Cancer.
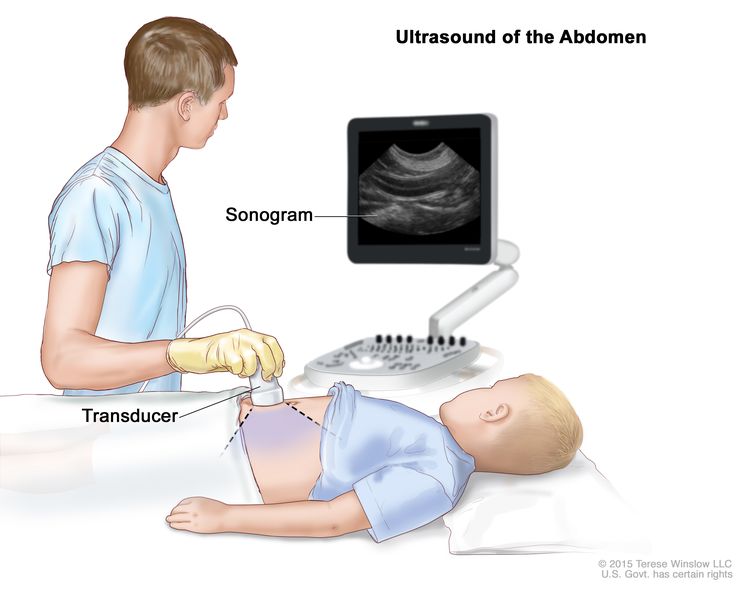
Ultrasound exam
An ultrasound exam uses high-energy sound waves (ultrasound) that bounce off internal tissues or organs and make echoes. The echoes form a picture of body tissues called a sonogram. An ultrasound exam of the abdomen to check the large blood vessels is usually done to help diagnose childhood liver cancer.
Chest x-ray
An x-ray is a type of high-energy radiation that can go through the body onto film, making a picture of areas inside the body. A chest x-ray is one that makes pictures of the lungs.
Immunohistochemistry
Immunohistochemistry uses antibodies to check for certain antigens (markers) in a sample of a patient's tissue. The antibodies are usually linked to an enzyme or a fluorescent dye. After the antibodies bind to a specific antigen in the tissue sample, the enzyme or dye is activated, and the antigen can then be seen under a microscope. This type of test is used to help diagnose cancer and to help tell one type of cancer from another type.
Getting a second opinion
You may want to get a second opinion to confirm your child's diagnosis and treatment plan. If you seek a second opinion, you will need to get medical test results and reports from the first doctor to share with the second doctor. The second doctor will review the pathology report, slides, and scans before giving a recommendation. This doctor may agree with the first doctor, suggest changes to the treatment plan, or provide more information about your child's cancer.
To learn more about choosing a doctor and getting a second opinion, visit Finding Cancer Care. You can contact NCI's Cancer Information Service via chat, email, or phone (both in English and Spanish) for help finding a doctor or hospital that can provide a second opinion. For questions you might want to ask at your child's appointments, visit Questions to Ask Your Doctor.
Prognostic factors for infantile choriocarcinoma of the liver
If your child has been diagnosed with infantile choriocarcinoma of the liver, you likely have questions about how serious the cancer is and your child's chances of survival. The likely outcome or course of a disease is called prognosis.
The prognosis for infantile choriocarcinoma of the liver depends on:
- the size of the tumor
- your child's health
- how the cancer responds to chemotherapy
- whether the cancer can be removed completely by surgery
- whether your child can have a liver transplant
- whether the cancer has just been diagnosed or has come back
For infantile choriocarcinoma of the liver that comes back after initial treatment, the prognosis depends on:
- where in the body the tumor recurred
- the type of treatment used to treat the initial cancer
No two people are alike, and responses to treatment can vary greatly. Your child's cancer care team is in the best position to talk with you about your child's prognosis.
Types of treatment for infantile choriocarcinoma of the liver
There are different types of treatment for children with infantile choriocarcinoma of the liver. You and your child's care team will work together to decide treatment. Many factors will be considered, such as your child's overall health and whether the cancer is newly diagnosed or has come back.
A pediatric oncologist, a doctor who specializes in treating children with cancer, will oversee treatment of infantile choriocarcinoma of the liver. The pediatric oncologist works with other health care providers who are experts in treating children with infantile choriocarcinoma of the liver and who specialize in certain areas of medicine. It is especially important to have a pediatric surgeon with experience in liver surgery who can send patients to a liver transplant program if needed. Other specialists may include:
Your child's treatment plan will include information about the cancer, the goals of treatment, treatment options, and the possible side effects. It will be helpful to talk with your child's care team before treatment begins about what to expect. For help every step of the way, visit our booklet, Children with Cancer: A Guide for Parents.
Surgery
When possible, the cancer is removed by surgery. The types of surgery that may be done are:
- Partial hepatectomy is surgery to remove the part of the liver where cancer is found. The part removed may be a wedge of tissue, an entire lobe, or a larger part of the liver, along with some of the healthy tissue around it. The remaining liver tissue takes over the functions of the liver and may regrow.
- Liver transplant is the removal of the entire liver by surgery, followed by a transplant of a healthy liver from a donor. A liver transplant may be done when the cancer is in the liver only, and a donated liver can be found. If the patient has to wait for a donated liver, other treatment is given as needed.
Chemotherapy is sometimes given before surgery to shrink the tumor and make it easier to remove. This is called neoadjuvant therapy.
Chemotherapy
Chemotherapy (also called chemo) uses drugs to stop the growth of cancer cells. Chemotherapy either kills the cancer cells or stops them from dividing. Chemotherapy may be given alone or with other types of treatment.
For infantile choriocarcinoma of the liver, the chemotherapy is injected into a vein. When given this way, the drugs enter the bloodstream and can reach cancer cells throughout the body.
Chemotherapy drugs used alone or in combination to treat infantile choriocarcinoma of the liver include:
Other chemotherapy drugs not listed here may also be used.
Learn more about how chemotherapy works, how it is given, common side effects, and more at Chemotherapy to Treat Cancer.
Clinical trials
For some children, joining a clinical trial may be an option. There are different types of clinical trials for childhood cancer. For example, a treatment trial tests new treatments or new ways of using current treatments. Supportive care and palliative care trials look at ways to improve quality of life, especially for those who have side effects from cancer and its treatment.
You can use the clinical trial search to find NCI-supported cancer clinical trials accepting participants. The search allows you to filter trials based on the type of cancer, your child's age, and where the trials are being done. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
Learn more about clinical trials, including how to find and join one, at Clinical Trials Information for Patients and Caregivers.
Treatment of infantile choriocarcinoma of the liver
Treatment of newly diagnosed infantile choriocarcinoma of the liver may include:
- chemotherapy to help shrink the tumor, followed by surgery to remove the tumor
- surgery to remove the tumor, followed by chemotherapy
- chemotherapy, followed by liver transplant if surgery to remove the tumor is not possible
Sometimes infantile choriocarcinoma of the liver continues to grow or recurs (comes back) after treatment. The cancer may come back in the liver or in other parts of the body. Your child's doctor will work with you to plan treatment if your child is diagnosed with recurrent infantile choriocarcinoma of the liver.
Side effects and late effects of treatment
Cancer treatments can cause side effects. Which side effects your child might have depends on the type of treatment they receive, the dose, and how their body reacts. Talk with your child's treatment team about which side effects to look for and ways to manage them.
To learn more about side effects that begin during treatment for cancer, visit Side Effects.
Problems from cancer treatment that begin 6 months or later after treatment and continue for months or years are called late effects. Late effects of cancer treatment may include:
- physical problems that affect hearing
- changes in mood, feelings, thinking, learning, or memory
- second cancers (new types of cancer)
Some late effects may be treated or controlled. It is important to talk with your child's doctors about the long-term effects cancer treatment can have on your child. Learn more about Late Effects of Treatment for Childhood Cancer.
Follow-up care
As your child goes through treatment, they will have follow-up tests or check-ups. Some of the tests that were done to diagnose the cancer or to find out the treatment group may be repeated to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your child's condition has changed or if the cancer has come back. To learn more about follow-up tests, visit Tests to diagnose infantile choriocarcinoma of the liver.
Coping with your child's cancer
When your child has cancer, every member of the family needs support. Taking care of yourself during this difficult time is important. Reach out to your child's treatment team and to people in your family and community for support. To learn more, visit Support for Families: Childhood Cancer and the booklet Children with Cancer: A Guide for Parents.