Anal Cancer Prevention (PDQ®)–Patient Version
What Is Prevention?
Cancer prevention is action taken to lower the chance of getting cancer. By preventing cancer, the number of new cases of cancer in a group or population is lowered. Hopefully, this will lower the number of deaths caused by cancer.
To prevent new cancers from starting, scientists look at risk factors and protective factors. Anything that increases your chance of developing cancer is called a cancer risk factor; anything that decreases your chance of developing cancer is called a cancer protective factor.
Some risk factors for cancer can be avoided, but many cannot. For example, both smoking and inheriting certain genes are risk factors for some types of cancer, but only smoking can be avoided. Regular exercise and a healthy diet may be protective factors for some types of cancer. Avoiding risk factors and increasing protective factors may lower your risk, but it does not mean that you will not get cancer.
Different ways to prevent cancer are being studied, including:
- Changing lifestyle or eating habits.
- Avoiding things known to cause cancer.
- Taking medicines to treat a precancerous condition or to keep cancer from starting.
General Information About Anal Cancer
Key Points
- Anal cancer is a disease in which malignant (cancer) cells form in the tissues of the anus.
- Squamous cell carcinoma is the most common type of anal cancer.
- In the United States, the number of new cases of anal cancer has increased in recent years.
Anal cancer is a disease in which malignant (cancer) cells form in the tissues of the anus.
The anus is the end of the large intestine, below the rectum. It is where stool (solid waste) leaves the body. The anus is formed partly from the outer skin layers of the body and partly from the intestine. The anus is connected to the rectum by the anal canal, which is about 1–1½ inches long. This area is controlled by two ring-like sphincter muscles, which open and close to let stool pass out of the body. 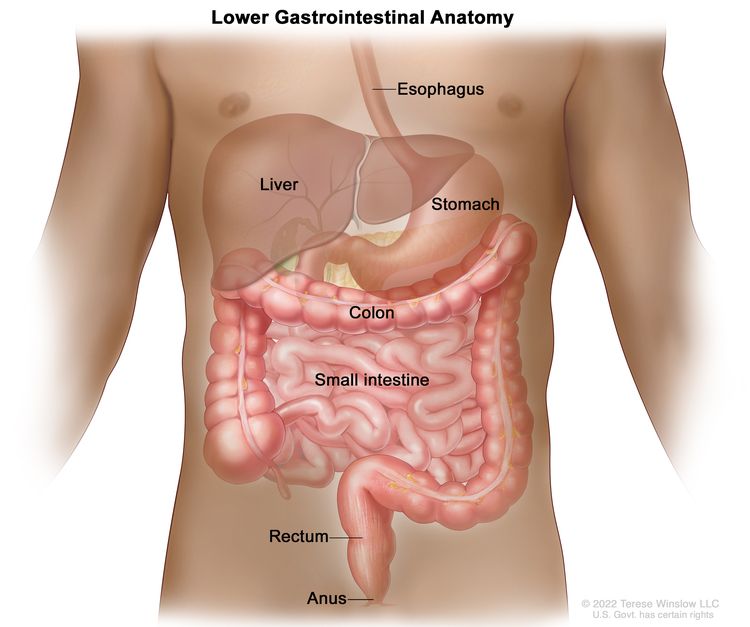
The skin around the outside of the anus is called the perianal area. Tumors in this area are skin tumors, not anal cancer.
To learn more about anal cancer, visit Anal Cancer Treatment.
Squamous cell carcinoma is the most common type of anal cancer.
In the United States, squamous cell carcinoma is the most common type of anal cancer. Studies show that human papillomavirus (HPV) infection is the main cause of this type of anal cancer.
Another type of anal cancer, called anal adenocarcinoma, is very rare and is not discussed in this summary.
In the United States, the number of new cases of anal cancer has increased in recent years.
Between 2012 and 2021, the number of new cases of anal cancer increased each year. Between 2013 and 2022, the rate of deaths from this disease also increased each year.
Anal Cancer Prevention
Key Points
- Avoiding risk factors and increasing protective factors may help prevent cancer.
- The following are risk factors for anal cancer:
- Anal HPV infection
- Certain medical conditions
- History of cervical, vaginal, or vulvar cancer
- HIV infection/AIDS
- Immunosuppression
- Certain sexual practices
- Cigarette smoking
- The following protective factors decrease the risk of anal cancer:
- HPV vaccination
- Screening for anal cancer using anoscopy
- Treatment of anal lesions
-
It is not clear if the following protective factor decreases the risk of anal cancer:
- Condom use
- Cancer prevention clinical trials are used to study ways to prevent cancer.
- New ways to prevent anal cancer are being studied in clinical trials.
Avoiding risk factors and increasing protective factors may help prevent cancer.
Avoiding cancer risk factors may help prevent certain cancers. Risk factors include smoking, having overweight, and not getting enough exercise. Increasing protective factors such as quitting smoking and exercising may also help prevent some cancers. Talk to your doctor or other health care professional about how you might lower your risk of cancer.
The following are risk factors for anal cancer:
Anal HPV infection
Being infected with human papillomavirus (HPV) is the main risk factor for anal cancer. Being infected with HPV can lead to squamous cell carcinoma of the anus, which is the most common type of anal cancer. About nine out of every ten cases of anal cancer are found in patients with anal HPV infection.
People with healthy immune systems are usually able to fight HPV infections. People with weakened immune systems who are infected with HPV have a higher risk of anal cancer.
Certain medical conditions
History of cervical, vaginal, or vulvar cancer
Cervical cancer, vaginal cancer, and vulvar cancer are related to HPV infection. Women who have had cervical, vaginal, or vulvar cancer have a higher risk of anal cancer.
HIV infection/AIDS
Being infected with HIV is a strong risk factor for anal cancer. HIV is the cause of AIDS. HIV weakens the body's immune system and its ability to fight infection. HPV infection of the anus is common among people who are HIV positive.
The risk of anal cancer is higher in men who are HIV positive and have sex with men compared with men who are HIV negative and have sex with men. Women who are HIV positive also have an increased risk of anal cancer compared with women who are HIV negative.
Studies show that intravenous drug use or cigarette smoking may further increase the risk of anal cancer in people who are HIV positive.
Immunosuppression
Immunosuppression is a condition that weakens the body's immune system and its ability to fight infections and other diseases. Chronic (long-term) immunosuppression may increase the risk of anal cancer because it lowers the body's ability to fight HPV infection.
People who have an organ transplant and receive immunosuppressive medicine to prevent organ rejection have an increased risk of anal cancer.
Having an autoimmune disorder, such as Crohn disease or psoriasis, may increase the risk of anal cancer. It is not clear if the increased risk is due to the autoimmune condition, the treatment for the condition, or a combination of both.
Certain sexual practices
The following sexual practices increase the risk of anal cancer because they increase the chance of being infected with HPV:
- Having receptive anal intercourse (anal sex).
- Having many sexual partners.
- Sex between men.
Men and women who have a history of anal warts or other sexually transmitted diseases also have an increased risk of anal cancer.
Cigarette smoking
Studies show that cigarette smoking increases the risk of anal cancer. Studies also show that current smokers have a higher risk of anal cancer than smokers who have quit or people who have never smoked.
The following protective factors decrease the risk of anal cancer:
HPV vaccination
HPV vaccines help protect the body against infection with certain types of HPV. They are used to prevent anal cancer, cervical cancer, vulvar cancer, vaginal cancer, and some other types of cancer caused by HPV. They are also used to prevent abnormal lesions caused by HPV that may lead to some of these cancers.
Studies show that being vaccinated against HPV lowers the risk of anal cancer. The vaccine may work best when it is given before a person is exposed to HPV.
Screening for anal cancer using anoscopy
Cancer screening is looking for cancer before a person has any symptoms. This can help find cancer at an early stage. When abnormal tissue or cancer is found early, it may be easier to treat.
An anoscopy is a procedure that uses a short, lighted tube called an anoscope to check for abnormal areas in the anus and lower rectum.
Studies suggest that using anoscopy to screen for anal cancer could reduce the number of deaths from the disease in people who are HIV positive.
Treatment of anal lesions
Studies show that treatment of anal high-grade squamous intraepithelial lesions (HSIL) decreases the development of anal cancer in people who are HIV positive.
It is not clear if the following protective factor decreases the risk of anal cancer:
Condom use
It is not known if the use of condoms protects against anal HPV infection. This is because not enough studies have been done to prove this.
Cancer prevention clinical trials are used to study ways to prevent cancer.
Cancer prevention clinical trials are used to study ways to lower the risk of developing certain types of cancer. Some cancer prevention trials include healthy people who may or may not have an increased risk of cancer. Other prevention trials include people who have had cancer and are trying to prevent recurrence or a second cancer.
The purpose of some cancer prevention clinical trials is to find out whether actions people take can prevent cancer. These may include eating fruits and vegetables, exercising, quitting smoking, or taking certain medicines, vitamins, minerals, or food supplements.
New ways to prevent anal cancer are being studied in clinical trials.
Information about clinical trials supported by NCI can be found on NCI’s clinical trials search webpage. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
About This PDQ Summary
About PDQ
Physician Data Query (PDQ) is the National Cancer Institute's (NCI's) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish.
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government’s center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about anal cancer prevention. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Updated") is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Screening and Prevention Editorial Board.
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become "standard." Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials can be found online at NCI's website. For more information, call the Cancer Information Service (CIS), NCI's contact center, at 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as “NCI’s PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary].”
The best way to cite this PDQ summary is:
PDQ® Screening and Prevention Editorial Board. PDQ Anal Cancer Prevention. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/anal/patient/anal-prevention-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389512]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 3,000 scientific images.
Disclaimer
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website’s E-mail Us.