Research in Early Detection of Lung Cancer
A great deal of research has been conducted in ways to find lung cancer early. Several methods are currently being studied to see if they decrease the risk of dying from lung cancer.
CT Scan
The NCI-supported National Lung Screening Trial (NLST) showed that low-dose CT scans can be used to screen for lung cancer in people with a history of heavy smoking. Lung cancer screening is generally recommended for people aged 50–80 years with a 20 pack year or more smoking history. Although the U. S. Preventive Services Task Force recommends screening only for those who currently smoke or quit within the last 15 years, some other medical groups now recommend screening regardless of when someone may have quit smoking
Markers in Blood and Sputum
Scientists are trying to develop or refine tests of sputum and blood that could be used to detect lung cancer early. Two active areas of research are:
- Analyzing blood samples to learn whether finding tumor cells or molecular markers in the blood will help diagnose lung cancer early.
- Examining sputum samples for the presence of abnormal cells or molecular markers that identify individuals who may need more follow-up.
Machine Learning
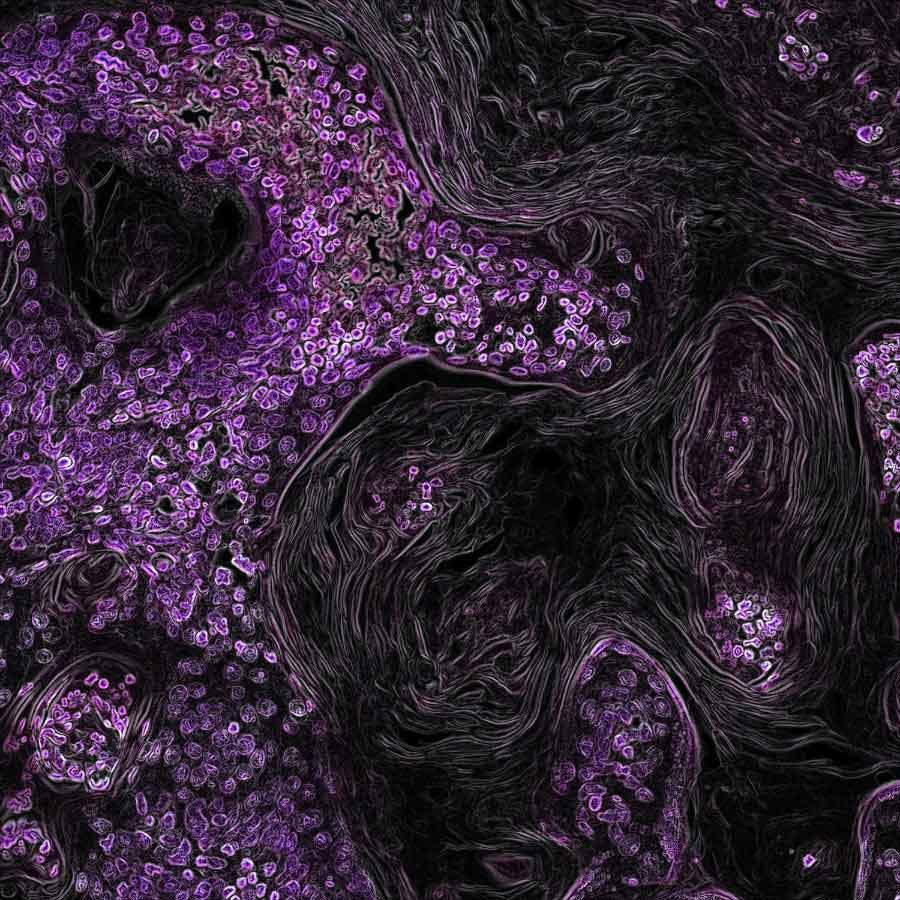
Machine learning is a method that allows computers to learn how to predict certain outcomes. In lung cancer, researchers are using computer algorithms to create computer-aided programs that are better able to identify cancer in CT scans than radiologists or pathologists. For example, in one artificial intelligence study, researchers trained a computer program to diagnose two types of lung cancer with 97% accuracy, as well as to detect cancer-related genetic mutations.
Research in Lung Cancer Treatment
Treatment options for lung cancer are surgery, radiation, chemotherapy, targeted therapy, immunotherapy, and combinations of these approaches. Researchers continue to look for new treatment options for all stages of lung cancer. Newer immunotherapies and targeted therapies are showing benefits, and researchers continue to improve these treatments for people with advanced lung cancer.
Because so many treatments have been developed that target specific alterations in NSCLC, all patients diagnosed with the disease should have their tumors tested for biomarkers to determine the best options for treatment.
Surgery
Early-stage lung cancer can often be treated with surgery. Researchers are developing approaches to make surgery safer and more effective. Surgery usually involves removal of an entire section (lobe) of the lung that contains the tumor. However, a recent clinical trial showed that, for certain people with early-stage NSCLC, removing a piece of the affected lobe is as effective as surgery to remove the whole lobe.
Immunotherapy
Immunotherapies help the body’s immune system fight cancer and are used to treat all stages of NSCLC. Still, these therapies are effective only in a minority of patients with the disease. Clinical trials are studying new combinations of immunotherapies with chemotherapy or other drugs to treat lung cancer.
Immunotherapies were initially used in people with advanced disease and continue to play a very important role in that setting. More recently, however, several immunotherapies have been shown to improve outcomes of people having surgery for early-stage disease:
- Atezolizumab (Tecentriq) and pembrolizumab (Keytruda) have been approved by the FDA as adjuvant treatments after surgery and chemotherapy, for some patients with early-stage NSCLC.
- Nivolumab (Opdivo) is approved to be used, along with chemotherapy, to treat patients with early-stage lung cancer before surgery (called neoadjuvant). This 2022 approval was based on a trial that showed patients at this stage who received neoadjuvant nivolumab plus chemotherapy lived longer than those who received chemotherapy alone.
- The FDA has approved the use of pembrolizumab plus chemotherapy before surgery, followed by pembrolizumab after surgery. One trial showed that patients with early-stage NSCLC who received this regimen had better outcomes than those who received just neoadjuvant or just adjuvant treatment.
To learn more, see Immunotherapy to Treat Cancer.
Targeted Therapies
Targeted therapies are now used as adjuvant therapy in people with lung cancer with certain genetic changes. In recent years, many targeted therapies have become available for advanced lung cancer, with more in development.
Anaplastic Lymphoma Kinase (ALK) Inhibitors
ALK inhibitors target cancer-causing alterations in a protein called ALK, which are found in 5% of people with NSCLC. Some of these treatments have shown to slow progression in those with brain metastases, which tends to occur in people with ALK alterations.
A study using the ALK inhibitor lorlatinib (Lorbrena) showed that people with advanced lung cancer went longer without their disease worsening than those who received a previously approved ALK inhibitor, crizotinib (Xalkori). Lorlatinib also slowed cancer progression in those with brain metastases.
Alectinib (Alecensa) was approved by the FDA in 2024 as adjuvant therapy for those with earlier-stage disease. A clinical trial showed that people treated with alectinib after surgery lived longer without a cancer recurrence than those treated with chemotherapy after surgery, the current standard treatment. In addition, cancer spread to the brain in far fewer people treated with alectinib than those who received chemotherapy.
These ALK inhibitors are improvements from previous ones in their enhanced ability to cross the blood–brain barrier. This progress is critical because in NSCLC patients with ALK alterations, disease progression tends to occur in the brain. Based on clinical trial results, in 2024 the FDA approved alectinib as adjuvant therapy for people with ALK-positive NSCLC.
EGFR Inhibitors
EGFR inhibitors block the activity of a protein called epidermal growth factor receptor (EGFR). Altered forms of EGFR, which are found at high levels in 10% to 15% of lung cancer patients in the United States, cause them to grow rapidly. Osimertinib (Tagrisso) is the most effective and most widely used EGFR inhibitor in advanced lung cancer.
Osimertinib was approved by the FDA in 2021 as adjuvant therapy after surgery for people with early-stage NSCLC with certain mutations in the EGFR gene. In addition to slowing disease progression, this treatment may improve how long people live.
For people with stage III EGFR-mutated NSCLC that cannot be removed by surgery, clinical trial results showed that treatment with osimertinib after chemotherapy and radiation therapy extended progression-free survival.
ROS1 Inhibitors
The ROS1 protein is involved in cell signaling and cell growth. A small percentage of people with NSCLC have rearranged forms of the ROS1 gene. Crizotinib (Xalkori) and entrectinib (Rozlytrek) are approved as treatments for patients with metastatic NSCLC who have these alterations. In late 2023, the FDA approved repotrectinib (Augtyro) for advanced or metastatic NSCLC with ROS1 fusions as an initial treatment and as a second-line treatment in those who previously received a ROS1-targeted drug.
BRAF Inhibitors
The B-Raf protein is involved in sending signals in cells and cell growth. Certain changes in the BRAF gene can increase the growth and spread of NSCLC cells.
The combination of the B-Raf-targeted drugs dabrafenib (Tafinlar) and trametinib (Mekinist), which targets a protein called MEK, has been approved as treatment for patients with NSCLC that has a specific mutation in the BRAF gene.
Encorafenib (Braftovi) combined with binimetinib (Mektovi) is approved for patients with metastatic NSCLC with a BRAF V600E mutation.
Other Inhibitors
Some NSCLC tumors have mutations in the genes NTRK-1 and NTRK-2 that can be treated with the targeted therapy larotrectinib (Vitrakvi). Those with certain mutations in the MET gene can be treated with tepotinib (Tepmetko) or capmatinib (Tabrecta). And those with alterations in the RET gene are treated with selpercatinib (Retevmo) and pralsetinib (Gavreto).
For people with advanced lung cancer that has mutations in the KRAS gene (about 25% of NSCLC cases) in whom immunotherapy and chemotherapy are no longer effective, several new options are available. These include sotorasib (Lumakras) and adagrasib (Krazati), which specifically target a protein made by the altered KRAS gene. Both slow progression of the disease, although neither has yet been shown to improve how long people live.
A 2023 clinical trial showed that, among people whose lung cancers have mutations in the RET gene, treatment with selpercatinib led to longer progression-free survival than treatment with chemotherapy or chemotherapy plus pembrolizumab.
View the full list of targeted therapies for lung cancer.
NCI-Supported Research Programs
Many NCI-funded researchers at the National Institutes of Health and across the United States and the world, are seeking ways to address lung cancer more effectively. Some research is basic, exploring questions as diverse as the biological underpinnings of cancer and the social factors that affect cancer risk. And some is more clinical, seeking to translate basic information into improved patient outcomes. The programs listed below are a small sampling of NCI’s research efforts in lung cancer.
- The Pragmatica-Lung Study is a randomized trial that will compare the combination of the targeted therapy ramucirumab (Cyramza) and the immunotherapy pembrolizumab (Keytruda) with standard chemotherapy in people with advanced NSCLC whose disease has progressed after previous treatment with immunotherapy and chemotherapy. In addition to looking at an important clinical question, the trial will serve as a model for future trials because it is designed to remove many of the barriers that prevent people from joining clinical trials.
- Begun in 2014, ALCHEMIST is a multicenter NCI trial for patients with early-stage NSCLC. It tests to see whether adding a targeted therapy after surgery, based on the genetics of a patient’s tumor, will improve survival.
- The Lung MAP trial is an ongoing multicenter trial for patients with advanced non-small cell lung cancer who have not responded to earlier treatment. Patients are assigned to specific targeted therapies based on their tumor’s genetic makeup.
- The Small Cell Lung Cancer Consortium was created to coordinate efforts and provide a network for investigators who focus on preclinical studies of small-cell lung cancer. The goal of the consortium is to accelerate progress on this disease through information exchange, data sharing and analysis, and face-to-face meetings.
- NCI funds eight lung cancer Specialized Programs of Research Excellence (Lung SPOREs). These programs are designed to quickly move basic scientific findings into clinical settings. Each SPORE has multiple lung cancer projects underway.
Clinical Trials
NCI funds and oversees both early- and late-phase clinical trials to develop new treatments and improve patient care. Trials are available for both non-small cell lung cancer treatment and small cell lung cancer treatment.
Lung Cancer Research Results
The following are some of our latest news articles on lung cancer research:
- Zenocutuzumab Approved to Treat Lung and Pancreatic Cancers with Rare Genetic Change
- Intensive Program Helps People Being Screened for Lung Cancer Quit Smoking
- Study Aims to Reduce Lung Cancer Stigma by Teaching Health Professionals Empathy
- Lorlatinib Slows Growth of ALK-Positive Lung Cancers, May Prevent Brain Metastases
- Durvalumab Extends Lives of People with Early-Stage Small Cell Lung Cancer
- Alectinib Approved as an Adjuvant Treatment for Lung Cancer
View the full list of Lung Cancer Research Results and Study Updates.