Technology - Cancer Currents Blog
News and commentaries on technology used to conduct cancer research, deliver cancer treatment, improve patient care, and screen for cancer, as well as other topics.
-
Rapid Genetic Test Could Help Guide Brain Cancer Surgery
Scientists have developed a test for use during brain cancer surgery that rapidly measures the levels of certain genetic mutations in patients’ tumor samples. The test uses droplet digital polymerase chain reaction technology and produces results within 15 minutes.
-
Will This Cancer Metastasize? Check Its “Stickiness”
A device that measures the “stickiness” of cancer cells in tumor samples may help predict the likelihood of a patient’s cancer metastasizing. Researchers believe the device could eventually help doctors make more informed treatment choices.
-
Are New Immune-Based Treatments for Kidney and Pancreatic Cancer on the Horizon?
In small trials, personalized treatment vaccines appeared to prevent cancer from returning in patients who had successful surgery to remove their tumors. The treatments, which were created based on intensive analyses of patients’ tumors, appeared to be safe.
-
Experimental Treatment Uses Engineered Fat Cells to “Starve” Tumors
Researchers have developed a form of cancer treatment that uses fat cells engineered to aggressively consume nutrients like glucose. When implanted in mice, the engineered cells appeared to outcompete tumors for nutrients, shrinking tumors.
-
Can AI Help Predict Which Cancer Patients Should Be Treated with Immunotherapy?
An AI-based tool called SCORPIO more accurately predicted whether cancer patients’ tumors would respond to checkpoint inhibitors than currently available tests, a new study found. It also predicted how long patients would live after treatment.
-
A “Living Medicine:” Engineered E. coli Shrink Tumors in Mice
In a pair of studies, researchers engineered a probiotic strain of E. coli called Nissle 1917 so it can help the immune system attack tumors. Although the E. coli were altered in different ways, resulting in two different immune-based treatment strategies, both were effective in mice.
-
Study Identifies Hundreds of Potential Targets for Cancer Drugs
Researchers have identified hundreds of promising targets for existing drugs or potential new cancer drugs. The findings relied heavily on proteogenomic data from more than 1,000 tumors representing 10 types of cancer released last year by NCI's CPTAC program.
-
To Combat Cancer Treatment Resistance, Researchers Try Leveraging Evolution
Scientists have developed a strategy for treating cancer that takes advantage of tumors’ ability to rapidly evolve and turns it against them. It involves intentionally making some tumor cells resistant to a specific treatment from the get-go.
-
How Breast Cancer Risk Assessment Tools Work
Drs. Ruth Pfeiffer and Peter Kraft of NCI’s Division of Cancer Epidemiology and Genetics discuss how breast cancer risk assessment tools are created and how people can use them to understand and manage their risk.
-
Experimental mRNA Vaccine Hints at Potential Against Glioblastoma
Recent results from several small clinical trials have suggested it may be possible to develop an effective immunotherapy for glioblastoma. Among them are findings from a four-patient trial testing a unique type of mRNA cancer vaccine.
-
Blood Test Accurately Detects Early-Stage Pancreatic Cancer
In a new study involving nearly 1,000 people, a liquid biopsy accurately detected early- and late-stage pancreatic cancer. When paired with a test for the protein CA19-9, the combination accurately identified 97% of people with early-stage disease.
-
First Cancer TIL Therapy Gets FDA Approval for Advanced Melanoma
In an event more than three decades in the making, FDA has approved lifileucel (Amtagvi), the first cancer treatment that uses immune cells called tumor-infiltrating lymphocytes, or TILs.
-
ctDNA May Guide Who Needs Chemo After Colorectal Cancer Surgery
Results from a new study suggest that the presence of circulating tumor DNA (ctDNA) in blood samples can predict which patients with colorectal cancer should and shouldn’t get chemotherapy after surgery to remove their tumors.
-
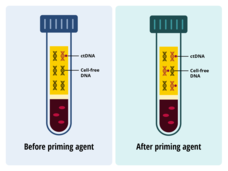
Pump Up the Volume: “Priming Agents” May Improve Cancer Liquid Biopsies
Using two different techniques, researchers showed they could temporarily boost ctDNA levels in the blood of mice with tumors. With more ctDNA in collected blood draws, a liquid biopsy could better detect cancer, the research team found.
-
FDA Authorizes Blood Test for Assessing Risk of Hereditary Cancers
The Food and Drug Administration (FDA) for the first time has granted marketing authorization for a blood test, the Invitae Common Hereditary Cancers Panel. The test detects inherited genetic changes that increase the risk of developing certain cancers.
-
Oncolytic Virus Enables the Immune System to Attack Tumors
A cancer-infecting virus engineered to tamp down a tumor’s ability to suppress the immune system shrank tumors in mice, a new study shows. The modified oncolytic virus worked even better when used along with an immune checkpoint inhibitor.
-
Is AI Ready to Play a Leading Role in Colorectal Cancer Screening?
Using computer-aided detection (CAD) during a colonoscopy doesn’t help doctors find the growths most likely to become colorectal cancer, two studies find. Researchers agreed that CAD, which is aided by artificial intelligence technology, needs further refinement.
-
Can Artificial Intelligence–Driven Chatbots Correctly Answer Questions about Cancer?
Can AI chatbots give people accurate information about cancer and its treatment? The answer appears to be: Not yet. Results from two studies have found that, although AI chatbots can gather cancer information from reputable sources, their responses to questions about treatment and other topics can include errors and omissions.
-
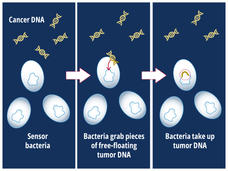
Could Bacteria Help Find Cancer?
Engineered bacteria can detect tumor DNA that has been shed into the gut by colorectal tumors, a new study in mice shows. The bacteria are programmed to seek and capture DNA containing a specific genetic change found in cancer.
-
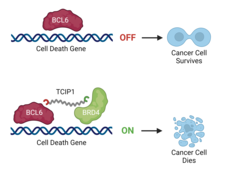
New Class of Compounds Rewires Cancer Cells to Self-Destruct
Researchers have created a molecule that, in cancer cells, hooks onto the protein BCL6 at one end and another protein that turns genes on at the other end. The result: self-destruct genes are turned up, causing the cancer cells to die.