How Some Brain Tumors Hijack the Mind to Grow
, by Sharon Reynolds
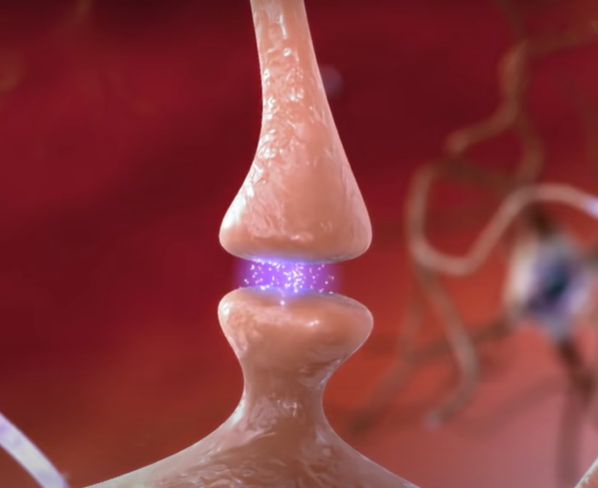
The brain’s incredible plasticity is what lets us think, learn, create, and remember. Throughout our lives, brain cells called neurons constantly form new connections, or synapses, that pass electrochemical signals from cell to cell. This ability, called neuroplasticity, underlies every function of the human mind.
But neuroplasticity may also have a dark side. In a new study, researchers found that an aggressive type of brain tumor called glioblastoma can co-opt the formation of new synapses to fuel its own growth. This neural redirection, they reported, also appears to play a role in the devastating cognitive decline seen in many people with glioblastoma.
But the research team also pinpointed a protein that appears to be critical to the hijacking process, and they showed that it may be a potential target for new treatments. The results were published May 4 in Nature.
Not all glioblastomas show this ability to remodel the brain to fuel tumor growth, explained the study’s senior investigator, Shawn Hervey-Jumper, M.D., of the University of California, San Francisco.
“But some [tumors] have found ways to exploit [neural] activity for their own benefit,” Dr. Hervey-Jumper said. “So now we have to think about strategies to decouple that [communication].”
In addition to potentially slowing glioblastoma growth, methods to break the lines of communication between tumor cells and neurons may help preserve patients’ cognitive function for longer, Dr. Hervey-Jumper added.
“That message resonates the most with patients and families that I’ve shared this work with,” he said.
Growing toxic neural connections
Tumors of the brain and central nervous system are rare overall. But glioblastoma is one of the most common of these rare tumors, and it’s also one of the deadliest. Glioblastoma is the most aggressive type of glioma: a class of tumors that arise from the supportive cells, most commonly astrocytes, that surround and protect neurons in the brain.
Treatments for glioblastoma—which can include surgery, radiation therapy, and chemotherapy—only keep the tumor at bay for a while, and most people live on average just over a year after a diagnosis.
But within this overall grim news hides much variation. While many peoples’ tumors are extremely aggressive, some are comparatively slow growing. Many factors influence an individual tumor’s aggressiveness.
Previous studies using cells and animal models of brain cancer had suggested that glioblastoma cells could affect how neurons behave, and that neuronal activity could, in turn, be one factor that promotes the aggressive growth of some tumors. But these phenomena hadn’t been documented in people.
“There is communication between normal astrocytes and neurons [in the human brain],” explained Mark Gilbert, M.D., of NCI’s Neuro-Oncology Branch, who was not involved in the study. “So for [tumor cells] to maintain some of that communicative interactivity is not outside the realm of possibility.”
Dr. Hervey-Jumper and his team, led by postdoctoral researcher Saritha Krishna, Ph.D., decided to look closely at how this cellular cross talk might work in people.
They started by taking recordings of the brain’s electrical activity in 14 people who were being prepared to undergo surgery for glioblastoma. Before the surgery, they placed electrodes that could record brain activity over language-processing regions of the brain that contained tumor cells, as well as adjacent brain tissue that didn’t harbor any tumor.
When the researchers recorded brain activity during simple language tasks completed by the patient (such as naming an object shown in a picture), they saw a boost of activity throughout the brain regions infiltrated by the tumor. These included areas not normally involved in speech production, suggesting that the tumor had triggered this neuroplasticity.
Specifically, the tumor appeared to have influenced neurons to make new connections in response to language in areas that normally wouldn’t produce such a response.
However, these new connections didn’t function as they should. Areas of the brain that had experienced this tumor-associated neuroplasticity struggled to process uncommon words compared with areas of the brain that hadn’t been invaded by the tumor.
So, while some glioblastomas appear to be capable of boosting the growth of new neural circuits, the research team concluded, this new connectivity may actually contribute to the cognitive decline seen in people with aggressive brain tumors.
Pinpointing a driver of damaging neuroplasticity
To better understand how some glioblastoma cells might be taking advantage of neuroplasticity, the researchers analyzed tissue samples taken from areas of people’s tumors that had high neural activity in response to language tasks and compared them to areas with low activity.
They found that a subset of tumor cells from areas with high functional connectivity and neuronal activity had an uptick in the expression of genes involved in assembling new neural circuits. This included a sevenfold increase in expression of a gene called THBS1, which directs cells to create a protein called TSP-1. TSP-1 is normally produced by healthy astrocytes in the brain and encourages the growth of new synapses.
Overall, about 2.5% of glioblastoma cells from the samples tested expressed THBS1, and cells from areas with high functional connectivity had higher levels of THBS1 expression than areas with low functional connectivity. Microscopy techniques confirmed that a subgroup of tumor cells in areas with high connectivity produced TSP-1, and that these areas formed more new synapses.
When the researchers grew neurons and tumor cells taken from either high connectivity or low connectivity areas together in lab dishes, tumor cells from high connectivity areas boosted the formation of new synapses and formed synapses with neurons themselves.
In contrast, tumor cells from areas with low connectivity did neither. But when the researchers added TSP-1, these tumor cells and neurons suddenly started to form connections.
Feeding off neural signaling
Additional experiments suggested that tumor cells from areas of high connectivity require neurons for their growth. Without the neurons, those same cells grew dormant.
The synapses formed between these tumor cells and neurons “aren’t true synapses—there’s not an electrical signal that’s then being transmitted to the next [tumor] cell,” explained Dr. Gilbert. “But it’s providing some sort of growth stimulus to that cell.”
The presence of neurons also made tumor cells from areas of high connectivity behave more invasively. For example, the team found that mice implanted with tumor cells derived from areas of high connectivity developed larger tumors and died sooner than mice implanted with tumor cells derived from areas of low connectivity.
The danger posed by tumors that manipulate neural connections seemed to hold for people as well.
When the researchers looked at 44 people with glioblastoma who had undergone surgery, those with tumors that showed many connections with surrounding neurons lived about a year less than people whose tumors lacked these connections (an average of 71 weeks versus 123 weeks). People whose tumors had high connectivity with surrounding neurons also had more trouble using language, a sign of worse overall cognitive functioning.
Turning a need into a target
There is a potential upside to the aggressiveness conferred by tumor–neuron communication, Dr. Gilbert explained.
“TSP-1 seems to be one of the main mediators [of this communication], which now gives you a potential [treatment] target,” he said.
Dr. Hervey-Jumper’s team agreed, and they reported promising results in experiments involving a drug called gabapentin, which blocks the activity of TSP-1.
In mice implanted with cells taken from high-connectivity glioblastomas, for example, treatment with gabapentin substantially decreased the rate at which tumors grew.
Gabapentin and several related drugs are already approved by the Food and Drug Administration for treating neurological conditions like epilepsy and some types of pain. Dr. Hervey-Jumper and his team are now planning a clinical trial to add gabapentin to standard treatment after surgery for glioblastoma, to see if the drug can improve both how long people live and their cognitive function.
Such an approach would likely only have potential benefit in people whose tumors are driven in part by high neural connectivity. Blood tests for TSP-1 could likely be used to identify patients who would be likely to benefit from a synapse-busting strategy, Dr. Hervey-Jumper explained.
More laboratory work is also needed to fully understand which comes first: tumor growth, or tumor–neuron connections, said Dr. Hervey-Jumper. While new connections may be driving tumor growth, it may also be that areas of the brain with more connections are simply more prone to developing tumors. Regardless of which comes first, the resulting cross talk remains a target worth exploring, he added.
"These two ghosts in the machine, the mind and the tumor, whispering to each other in the dark recesses of the brain, engage in a conversation that could be well worth eavesdropping on," George Ibrahim, M.D., Ph.D., of the Hospital for Sick Children in Toronto, and Michael Taylor, M.D., Ph.D., of the Texas Children's Cancer Center, wrote in an editorial that accompanied the new paper.
"Doing so,” they continued, “could lead to innovative approaches to improving the lives of people with brain tumors."