Colonoscopy after Positive FIT Test Cuts Risk of Colorectal Cancer Death
, by Elia Ben-Ari
New research underlines the importance of following up with a colonoscopy exam after a positive (abnormal) result on an at-home stool test to screen for colorectal cancer. The test, known as the fecal immunochemical test (FIT), checks for traces of blood in patient-collected stool samples, which can be an early sign of cancer.
Screening for colorectal cancer, the second leading cause of cancer-related deaths in the United States and other high-income countries, has been shown to reduce deaths from this disease.
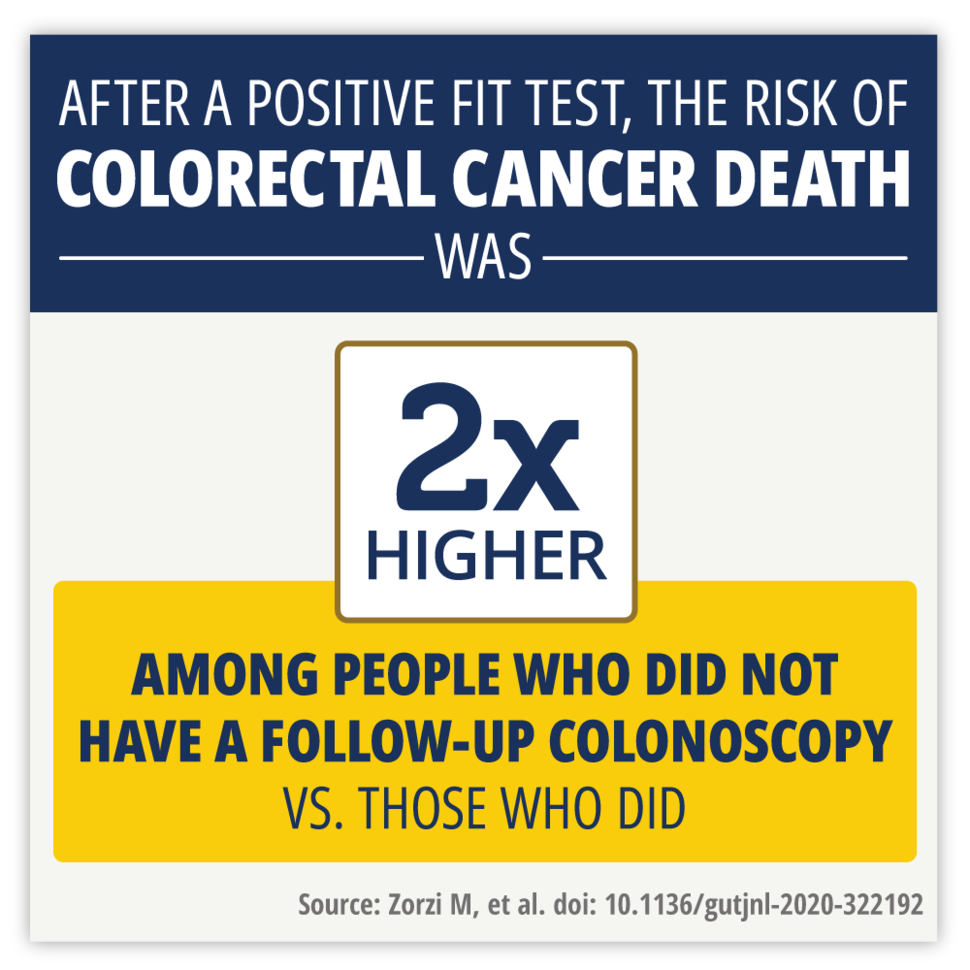
In the new study, researchers found that people who had a positive FIT result (signs of blood in the stool) but did not have a follow-up colonoscopy were twice as likely to die as those who did have a follow-up colonoscopy.
“This study emphasizes that cancer screening is really a process, not a single step, and shows the importance of completing all steps of the process,” said gastroenterologist Douglas Corley, M.D., Ph.D., of Kaiser Permanente, Northern California, who was not involved in the study.
Until now, there hasn’t been much information on how a lack of follow-up testing after a positive FIT result may affect people’s risk of dying from colorectal cancer, Dr. Corley noted. Findings from the study, which was conducted in Italy, were published March 31 in Gut.
“The study points to the importance of more closely monitoring people who do not follow recommendations after a positive FIT result,” said Erica Breslau, Ph.D., M.P.H., of NCI’s Healthcare Delivery Research Program, who also was not involved in the study. The findings also highlight the need to “identify opportunities to improve what is currently being done” to ensure that people get the follow-up tests they need, Dr. Breslau said.
FIT is one of the most widely used colorectal cancer screening tests worldwide. Experts generally recommend that people repeat this test every 1 to 2 years. People with a positive FIT test result are advised to have a colonoscopy to investigate the cause of the bleeding because a FIT test alone cannot diagnose cancer.
A follow-up, or diagnostic, colonoscopy can find not only colorectal cancer but also precancerous growths, or polyps, that doctors can remove during the procedure, reducing the risk of future cancers. If cancer is detected, treatment is usually the next step.
Many successful colorectal cancer screening programs, including those in the United States, use some combination of stool-based tests, such as FIT, and screening colonoscopy, Dr. Corley said, so the new study results “are very relevant to settings in the United States.”
Delayed diagnosis of colorectal cancer leads to higher risk of death
For the study, Manuel Zorzi, M.D., M.Sc., of the Veneto Tumour Registry in Padua, Italy, and his colleagues, examined the medical records of participants in a regional colorectal screening program who took a FIT test between January 1, 2004, and September 30, 2017.
The program offers free FIT testing once every 2 years to people 50–69 years old. Stool samples collected at home are sent in for analysis. People with a positive FIT result are contacted by phone by trained individuals and a follow-up colonoscopy exam is offered free of charge.
The study included 111,423 people who had a positive FIT test, of whom 88,013 people had a follow-up colonoscopy as part of the program (colonoscopy group) and 23,410 did not (no-colonoscopy group). Nearly all of the people who had a follow-up colonoscopy did so within a year of the positive FIT result.
The researchers compared the numbers of new colorectal cancer cases diagnosed, deaths from colorectal cancer, and deaths from any cause in the two groups over time for up to 10 years after an initial positive FIT result.
During the study period, fewer than 1% of people in each group died of colorectal cancer. However, those who did not get a follow-up colonoscopy were about twice as likely to die of colorectal cancer over a 10-year period as those who did have a follow-up colonoscopy.
In the colonoscopy group, the number of new colorectal cancers diagnosed went up sharply in the first 6 months or so after a positive FIT result and leveled off after that.
The initial sharp rise was expected, the researchers noted, due to colorectal cancer being found during follow-up colonoscopy. The low incidence of colorectal cancer after that was likely due to the early detection of cancers and the removal of precancerous lesions during colonoscopy, Dr. Breslau explained.
“This demonstrates the longer-term protective value of completing the screening process, which is another new piece of information provided by the study,” Dr. Corley said.
By contrast, in the no-colonoscopy group, new cases went up more gradually but continued rising over 10 years. People in this group were more likely to have their cancer detected only after symptoms appeared, when the cancer was more advanced. This delayed diagnosis likely explains the higher death rate from colorectal cancer in this group, Dr. Breslau said.
Room for improvement
Many colorectal cancer screening programs, including some in the United States, “struggle to ensure timely colonoscopy completion among those with a positive FIT, with rates as low as 50%,” Dr. Zorzi and his colleagues wrote. But the program in northeast Italy, which started in 2002, has maintained colonoscopy rates of 80% at just 3 months after a positive test result, they noted.
This follow-up rate “is comparable to some of the best follow-up rates in the United States and elsewhere,” Dr. Corley said.
Yet there’s clearly room for improvement.
“This study doesn’t help us understand why people aren’t following up,” Dr. Corley said. “Understanding why some people are willing to be screened but do not follow up can lead to improvements in the effectiveness of the screening process.”
Multiple factors can contribute to people not getting follow-up colonoscopy exams, both he and Dr. Breslau said.
In the United States, cancer screening is a complex process that involves multiple steps and can be affected by many factors, Dr. Breslau said. Such factors include the patient’s personal circumstances (for example, access to transportation), whether they have health insurance, whether they can get timely access to colonoscopy, and whether they have had an adequate conversation with their doctor about screening.
“In Italy, unlike in the United States, all citizens are entitled to care that is mostly free through Italy’s National Health Service. This study shows that even with a national health service that provides universal coverage, there are other barriers to obtaining care,” Dr. Breslau said. For example, people’s fears about the preparation for colonoscopy continue to be a major barrier.
Dr. Zorzi’s team found that people in the no-colonoscopy group were at higher risk of dying from all causes, not just from colorectal cancer. This points to one possible reason why people in this group, on average, were less likely to get follow-up colonoscopy exams, Dr. Corley said.
“Some people may have had other illnesses that precluded them from having a colonoscopy or made them feel that they were more likely to die from causes other than colorectal cancer,” he explained.
The ongoing NCI-funded PROSPR program aims to better understand how to improve the cancer screening process and reduce disparities in colorectal and other cancer screening in community health care settings in the United States.
Dr. Corley, who is the lead investigator for the colon cancer component of PROSPR, stressed the effectiveness of colorectal cancer screening.
“One study we published showed that by increasing screening rates from 40% to 80%, we could cut the incidence of colorectal cancer deaths in half,” he said. “[This] raises the importance of being able to get the individual steps correct and completed as best you can ... because every step where you lose some people in follow-up can have a big impact.”