For Common Form of Bladder Cancer, Chemo Combo Effective Alternative to BCG
, by Carmen Phillips
Long before the COVID pandemic–fueled supply chain crisis, there was a shortage of a cancer therapy called BCG that’s used to treat the most common form of bladder cancer. BCG has long been the go-to initial treatment for a form of the disease called high-risk non-muscle-invasive bladder cancer (NMIBC).
The continuing BCG shortage has forced doctors to rely on other treatments for their patients with high-risk NMIBC. Among the alternatives they have turned to is a combination of two chemotherapy drugs, gemcitabine and docetaxel. And researchers from the University of Iowa have now published results from the largest study to date of people with high-risk NMIBC treated with this combination.
Overall, they reported, 82% of people who received periodic treatment with both drugs after surgery to remove their bladder tumor were still alive 2 years later without the cancer returning. The findings were published July 27 in the Journal of Urology.
None of the more than 100 patients in the study died from bladder cancer during the study period, and side effects from the drugs, which are delivered directly into the bladder, were largely minor.
The results with the chemotherapy combination were “similar to, or even somewhat better, than what is typically seen in patients treated with BCG,” said the study’s lead investigator, Vignesh Packiam, M.D., of the University of Iowa Health Care Department of Urology. “We’re very excited to have this treatment option for patients who would otherwise be left without an effective alternative.”
There was broad agreement among urologic oncologists that the findings show the chemo combination is an excellent option when BCG is not available.
The study’s findings “will be extremely helpful for the urologist to discuss with patients when BCG is not available, as all patients want to know how their outcomes could be affected by the BCG shortage,” wrote Joshua Meeks, M.D., Ph.D., a urologic oncologist at Northwestern University’s Feinberg School of Medicine, and colleagues in an accompanying editorial.
Sandeep Gurram, M.D., of the Urologic Oncology Branch in NCI’s Center for Cancer Research, called the findings “very promising.” In particular, Dr. Gurram noted that the combination appeared to work well even in people with the most concerning types of high-risk NMIBC.
He cautioned, however, that this study had important limitations and is not the final word on the treatment of high-risk NMIBC, regardless of BCG’s availability. For example, it wasn’t a clinical trial that directly compared BCG with gemcitabine and docetaxel.
Several ongoing and soon-to-be-launched clinical trials should help address some of the most important outstanding questions, he noted.
From BCG to chemo combos
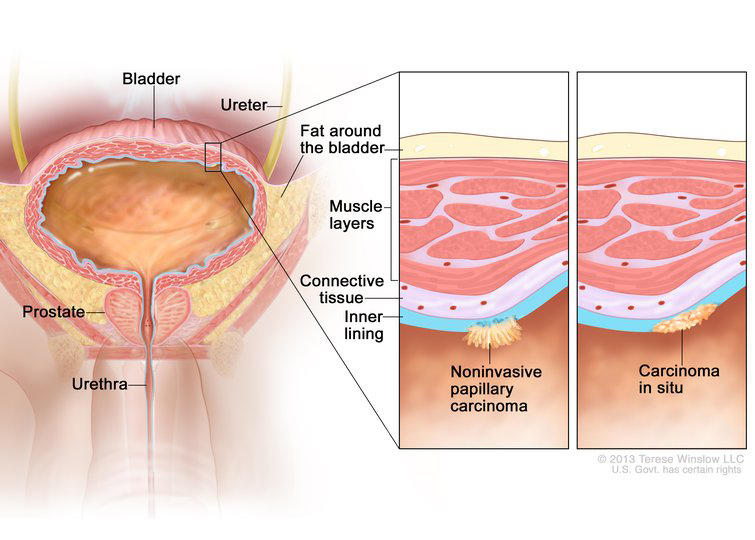
Non-muscle-invasive bladder cancer is so called because the tumor resides strictly in the bladder’s interior lining, called the mucosa. Among other tasks, this mucosal lining operates as a barrier between the smooth muscle that encases the bladder and the urine within it.
About 70%–75% of bladder cancer diagnoses are NMIBC and about 25% of these are at high risk of progressing to muscle-invasive bladder cancer.
A tumor is called high-risk when its size or other features suggest that it’s biologically aggressive. One form of high-risk NMIBC, for example, is called carcinoma in situ, in which the tumor spreads along the mucosa in a pancake-like shape. These tumors are not only aggressive, Dr. Packiam explained, but particularly resistant to treatment with BCG. And when they do come back, it’s often in a more invasive form.
The treatment course for high-risk NMIBC begins with removing the bladder tumors via a surgical procedure called TURBT. Surgery is followed by additional treatments, known as adjuvant therapy, to kill off any remaining cancer cells and reduce the risk of the cancer coming back.
For most people with NMIBC, if no additional treatment is given after surgery, the disease often recurs at some point. So the primary goal of adjuvant therapy is to prevent recurrences for as long as possible and also to prevent recurrences from invading into the bladder, Dr. Packiam said. Tumors that invade to the muscle wall of the bladder require more aggressive surgery, including potentially removing the bladder entirely.
For decades, adjuvant therapy with BCG—a severely weakened form of a bacterium that was originally developed as a tuberculosis vaccine—was “the gold standard for preventing progression and recurrence” in high-risk NMIBC, he explained.
But starting in the early 2010s, supplies of BCG started to run short after one of the two companies that produced it stopped doing so. Only Merck now manufactures BCG for use in the United States. And according to the company, manufacturing issues as well as increased global demand continue to limit its availability.
Last year, the company announced that it was building a new manufacturing facility for BCG, allowing the company to triple its output of the therapy. However, BCG supply isn’t expected to recover for at least several more years.
Single chemotherapy drugs have been among the most common alternatives used during the BCG shortage, Dr. Packiam said. But they have been shown to have decreased effectiveness against high-risk NMIBC.
Combinations of chemotherapy drugs have proven to be effective in people with high-risk NMIBC whose cancer comes back after BCG treatment, Dr. Gurram said. So it made sense, he continued, to study chemotherapy combinations as an initial, or first-line, treatment.
Promising recurrence-free survival
Michael O’Donnell, M.D., another member of the University of Iowa research team, pioneered the use of the gemcitabine–docetaxel combination to treat high-risk NMIBC not long after the BCG shortage began.
So for this study, the team looked back in time at data from patients who received adjuvant treatment with the chemo combination at their hospital. The data review covered patients treated from May 2013, about 1 year after the BCG shortage started, through April 2021.
Patients in the study initially received both drugs—each one delivered separately via a catheter directly into the bladder—once a week for 6 weeks (induction therapy). If there were no serious problems with side effects or the cancer did not come back, patients then got both drugs once a month for up to 2 years (maintenance therapy). The analysis included 107 people and the median follow-up was 15 months.
| Time after starting treatment | Patients alive without their cancer returning |
| 6 months | 89% |
| 12 months | 85% |
| 24 months | 82% |
In addition to more than 80% of patients remaining alive without their cancer returning at 2 years, only one patient in the study had to go on to surgery to have their bladder removed. The most common side effect was having to urinate frequently and often feeling the urge to urinate.
Dr. Packiam acknowledged that the study has several limitations. Among them was that the study looked back in time, all of the patients were treated at the same hospital, and nearly all patients in the study were White.
All of these things may limit how applicable the findings are to the broader US population. “Absolutely, larger studies in more diverse populations are needed,” he said. However, he continued, the BCG shortage created a situation where doctors and their patients had no choice but to use something else.
“Iowa has been seriously affected by the [BCG] shortage. We have very little supply here,” Dr. Packiam said. “So we really have come to rely on this [combination].”
More definitive answers on the horizon
One of the most important takeaways from the study, Dr. Gurram said, is that the gemcitabinedocetaxel combination appeared to work well in all high-risk patients, including those with carcinoma in situ.
Is using less BCG okay?
Researchers are investigating another potential solution to the BCG shortage: using a lower dose of BCG per treatment. Several studies have suggested that using a lower dose may be a suitable option, including a study published last year showing that, in people with high-risk NMIBC, using one-third of the standard dose of BCG didn’t appear to be any less effective than the standard full dose.
The study had a large population of people with high-risk tumors “that are often resistant to BCG and they are still getting very good [recurrence-free survival] numbers,” he said.
Nevertheless, evaluating how the combination performs in people from different racial and ethnic backgrounds will be important.
“We’ve seen time and again that something can perform well in [retrospective studies], but once it gets to the community, we can see differing results,” Dr. Gurram said.
The need to travel to the hospital monthly to get the maintenance treatment is a challenge of this particular regimen, Dr. Packiam noted. That’s particularly true in rural areas and for people without easy access to transportation.
“It does produce some logistical burdens for patients,” he said.
Along those lines, Dr. Meeks and his colleagues wondered about the extent to which maintenance therapy is even needed. As with BCG treatment, over time, many patients stop taking it. So “it will be important to determine if 6, 12 or 24 months of [gemcitabine and docetaxel] is necessary,” they wrote.
In the meantime, Dr. Gurram said, researchers are looking more carefully at existing and potential new treatments for high-risk NMIBC.
For example, a large NCI-supported trial that will randomly assign patients to either BCG or the docetaxel–gemcitabine combination is in the works but hasn’t yet launched. And a series of clinical trials are underway testing BCG in combination with immunotherapy drugs for patients with high-risk NMIBC.
Dr. Gurram said he’s hopeful that newer therapies can further improve treatment of NMIBC across the board.
“But, honestly, revisiting old chemotherapies that give promising results is great to see.”