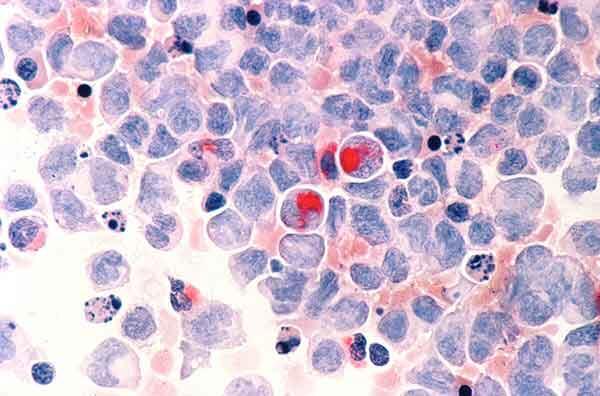
Two New Therapies Approved for Acute Myeloid Leukemia
, by NCI Staff
The Food and Drug Administration (FDA) recently approved two new treatments for some adult patients with acute myeloid leukemia (AML): enasidenib (Idhifa®), a drug that targets aberrant forms of the IDH2 protein; and liposomal cytarabine-daunorubicin CPX-351 (Vyxeos™), a two-drug chemotherapy combination encapsulated in tiny fatlike particles called liposomes.
The Vyxeos approval, announced on August 3, is for patients with either of two high-risk forms of AML. The enasidenib approval, announced two days earlier, is for adults with AML whose tumors have mutations in the IDH2 gene as detected by an FDA-approved test and whose disease has returned after earlier treatment (relapsed) or did not respond to standard treatments (refractory).
An estimated 10–15% of adults with AML have cancer-causing IDH2 mutations. Enasidenib, which is taken by mouth, is the first IDH-targeted drug approved by FDA.
FDA also approved a companion diagnostic test, the RealTime™ IDH2 assay, to detect IDH2 mutations and identify patients who could benefit from the drug. The enasidenib approval “is an advance in precision medicine for AML,” said Richard Little, M.D., of NCI’s Division of Cancer Treatment and Diagnosis.
Notable Results but More to Learn
Enasidenib’s approval was based on the results of a single-arm clinical trial that enrolled 199 patients. All patients in the trial had relapsed or refractory AML and an IDH2 mutation detected by the RealTime test, and all were treated with enasidenib.
In particular, FDA based its approval on the rates and durations of two outcomes: complete response and complete response with partial hematologic recovery (CRh), which means that no signs of leukemia are found but some of the blood counts, or just the platelet count, have not returned to normal levels. The agency also cited the finding that 34% of patients who, at trial entry, required red blood cell and/or platelet transfusions no longer needed transfusions during at least one 56-day period while on enasidenib.
Common side effects of the drug included jaundice and nausea. A serious side effect known as differentiation syndrome, which includes fever and respiratory distress and can be fatal if not treated, occurred in 14% of patients.
Detailed data from the phase I/II clinical trial of enasidenib showed that, overall, 40% of study participants responded to enasidenib and 19% experienced a complete remission of their leukemia.
The published results also showed that median overall survival was 9.3 months from the start of treatment with the study drug among all patients in the trial, and 19.7 months among those patients who attained complete remission.
FDA’s approval of a treatment based on results of a single-arm phase II trial is notable, Dr. Little said. The response and overall survival rates seen in the trial are better than what is typically seen with existing treatments for adults with relapsed or refractory AML, he added.
“In this setting, where patients have a high risk of treatment failure based on already having recurrent leukemia, a complete response of more than 8 months is a long time,” especially with a single targeted therapy, Dr. Little noted.
A remission of that length would allow planning and decision-making about other therapies, such as allogeneic stem cell transplantation, which can be curative for AML, he said.
Dr. Little stressed that “there is much more to learn” about enasidenib. “The challenge will be to investigate the use of this agent in patients with newly diagnosed AML and IDH2 mutations, and to learn how to combine the drug with other AML treatments to make a substantial difference in patient outcomes,” he said.
Liposome-Based Treatment Is a New Standard of Care
On the heels of the enasidenib approval, FDA approved Vyxeos for adults with two types of AML that have a particularly poor prognosis—newly diagnosed AML that develops after treatment for another type of cancer (t-AML), and AML with myelodysplasia-related changes (AML-MRC).
Vyxeos consists of a combination of two anticancer drugs, daunorubicin and cytarabine, encapsulated in a liposome—a tiny fatlike particle. The liposomes were designed to provide optimal delivery of a specific ratio of the two drugs that has been shown in lab experiments to have a greater combined effect than when each drug is given alone.
And because cancer cells tend to take up liposomes more efficiently than do other cells, the dose of the drugs that is delivered into leukemia cells is higher than that seen by normal cells, possibly enhancing the therapeutic effect without increasing toxicity, Dr. Little explained.
The FDA approval was based on results of a phase III clinical trial that randomly assigned patients 60–75 years of age to Vyxeos or the standard combination regimen of daunorubicin and cytarabine (known as 7+3), in which the two drugs are given separately.
Results of the trial, presented at the 2016 American Society of Clinical Oncology annual meeting, showed that median overall survival was 9.6 months in patients who received Vyxeos, compared with 5.9 months in the control group. The complete response rate was 38% in the Vyxeos-treated group and 26% in the control group. A greater proportion of patients in the Vyxeos group (34%) than in the control group (25%) went on to have a stem cell transplant.
Side effects in the two treatment groups were similar. The most common serious side effects included difficulty breathing, bleeding events, fever with low white blood cell count, and abnormal heart rhythms.
According to FDA, the approval is the first specifically for newly diagnosed t-AML and AML-MRC.
The liposome-based formulation “will be viewed as a new standard of care for older patients with these forms of high-risk AML,” Dr. Little said.
As with enasidenib, “more work will need to be done to fully inform using Vyxeos outside [of] the types of patients who were included in this clinical trial,” Dr. Little noted. “The temptation will be to use the liposomal preparation in patients with other high-risk forms of AML, and in my view, we need more information before we know whether that will improve outcomes for these patients.”