Dual-Biomarker Blood Test Shows Promise for Pancreatic Cancer Early Detection
, by NCI Staff
A new blood test may be able to accurately detect pancreatic cancer at its earliest stages, when it is most likely to respond to treatment, findings from a new study suggest.
In an early-phase study, the test, which measures the levels of two specific proteins in blood, distinguished tissue samples from patients with pancreatic cancer from samples from people without the disease and samples from people with noncancerous pancreatic conditions, such as pancreatitis.
The study, published July 12 in Science Translational Medicine, included multiple steps to confirm that the approach was accurate and feasible for the detection of pancreatic cancer. Even so, the authors stressed, further research is needed to refine the test, which they believe should be used only in people at high risk for the disease.
The research team has “additional biomarkers that we want to test to improve” the test’s performance, explained the study’s senior investigator, Ken Zaret, Ph.D., of the University of Pennsylvania Abramson Cancer Center. “But that will take several years to develop.”
Early Detection Lacking
Despite being relatively rare in the United States, pancreatic cancer is among the leading causes of cancer death. By the end of the decade, in fact, it is projected to be the second leading cause of cancer death behind lung cancer.
Pancreatic cancer’s high mortality rate is due in large part to the fact that it’s typically detected at an advanced stage, by which time it has spread from the pancreas to nearby lymph nodes and other organs. At this point, the cancer can’t be removed by surgery and doesn’t respond well to chemotherapy and radiation. Five-year survival for those diagnosed with advanced disease is less than 10%.
Previous efforts to develop ways to detect pancreatic cancer at an early stage have been unsuccessful, although more recently some have shown promise. Many of the previous early-phase studies that identified potential markers to detect the disease before it has spread relied on tumor samples from patients with advanced-stage disease or on human cell lines of advanced disease, Dr. Zaret said.
As a result, he continued, there were few “good human cell models for accessing live cells from early-stage tumors that we can study for secreted and released markers.”
Discovering Biomarkers with an ‘Unusual’ Model
For their study, which was funded in part by NCI, Dr. Zaret and his colleagues conducted a lengthy, multistep biomarker discovery and validation process.
The first step, known in biomarker research as the discovery phase, was to identify potential biomarkers for early detection. Later activities, known as the validation phase, focused on confirming whether the biomarkers identified in the discovery phase accurately identified cancer when analyzed in a larger group of samples.
The process for conducting the study was thorough and well thought-out, said Sudhir Srivastava, Ph.D., who heads the Early Detection Research Network in NCI’s Division of Cancer Prevention. “The investigators took a meticulous approach to this study and the results are very encouraging,” he said.
Early Detection of Pancreatic Cancer Focus of NCI-Supported Consortium
The Penn and Mayo Clinic research team that led this study are one of seven groups in the NCI-funded Pancreatic Cancer Detection Consortium (PCDC). The PCDC was developed following the enactment of the Recalcitrant Cancer Research Act of 2012, based on recommendations from an NCI-convened workshop on pancreatic cancer.
Each of the seven PCDC groups are focused on finding ways to identify pancreatic cancer at its earliest stages, when it is much more amenable to treatment. This research includes developing and testing new biomarkers that can identify early-stage pancreatic cancer or precancerous pancreatic lesions, and identifying people who are at high risk of developing pancreatic cancer who are candidates for early intervention.
For the discovery phase, the research team relied on a cell line they developed previously by “reprogramming” cells from an advanced human pancreatic tumor to become what are known as induced pluripotent stem cell (iPSC)-like cells—meaning that the cells have mostly regained the properties for forming different cell types.
In what Dr. Zaret called an “unusual” cancer model, these reprogrammed cells, once transplanted into mice, form precancerous pancreatic lesions within 3 months that, by 6 to 9 months, progress to invasive pancreatic tumors. The tumors that form in the mice have many of the genetic hallmarks of pancreatic cancer, such as mutations in the KRAS and TP53 genes, he said.
“We put a lot of work up front into developing this model … to try to rigorously recapitulate how human pancreatic cancer progresses, and then did our discovery from that,” he explained.
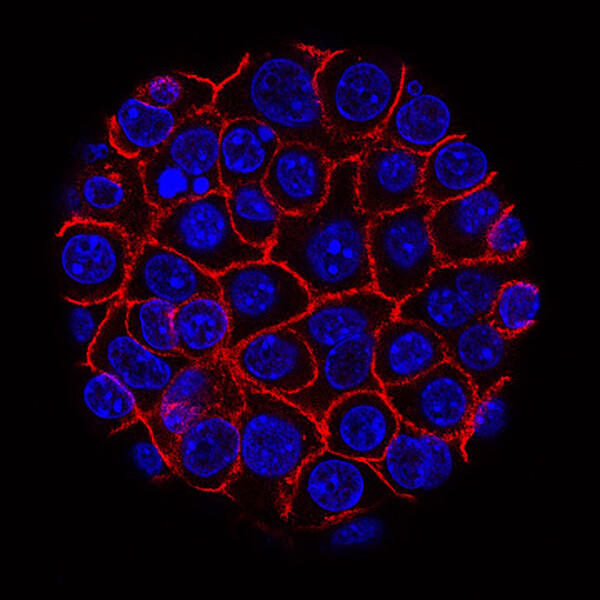
The researchers took samples from the precancerous lesions (known as PanIN2 and PanIN3) and the tumors that formed in the mice, grew them in the laboratory so they would form 3D organ-like spheres called organoids, and analyzed the organoids to identify the proteins that they secreted. They identified more than 100 secreted proteins, nearly half of which are known to be part of an important signaling pathway in pancreatic cancer called TGFβ.
Of these proteins, they zeroed in on three that are known to be central components of the TGFβ signaling pathway and for which there were reliable commercial tests.
Validate, Validate, and Cross Validate
The validation phase included multiple independent investigations. Beginning with high-quality plasma samples from 10 patients with pancreatic cancer and 10 carefully matched control individuals without disease (both supplied by study coauthor Gloria Petersen, M.D., of the Mayo Clinic), they found that elevated levels of only one of the three proteins, THBS2, accurately and reliably discriminated between the patient samples and those from healthy controls.
Confirmation of the potential importance of THBS2 came when they looked at data from The Cancer Genome Atlas, which showed that THBS2 levels were much higher in pancreatic tumors than nearly all other tumor types.
The next phase of the validation involved testing for THBS2 in two larger collections of human plasma samples (189 and 537, respectively). These collections included a broader array of samples, including from patients with early- and late-stage pancreatic cancer, healthy individuals, and patients with a history of chronic pancreatitis.
Again, measuring THBS2 levels accurately distinguished the samples from patients with pancreatic cancer from the non-cancer samples. Plasma levels of a protein biomarker already used to track the progression of pancreatic cancer, CA19-9, also demonstrated similar accuracy, they reported.
When THBS2 and CA19-9 levels were assessed in combination, the two markers were more accurate at differentiating between cancer samples and noncancer samples than either marker alone, the researchers reported. The accuracy held up regardless of whether the samples were from patients with early-stage or more advanced tumors.
They then refined the testing approach to identify the levels of the two markers that would most accurately detect cancer, settling on levels that provided 99% specificity (negative results among persons without disease), and 87% sensitivity (positive results among persons with disease).
The combination of the two markers proved to be better than either of the markers alone, they explained, because often when the level of one marker was low in a plasma sample, the level of the other marker was high.
“Thus, the two markers appeared to be complementary in their ability to detect pancreatic cancer,” the team wrote.
Testing for both markers in plasma relies on a commonly used technology called ELISA, which uses antibodies that are specific to certain proteins to detect and measure the amount of that protein in the blood sample. The testing was done over several years, using different ELISA kits on the same samples, to confirm that the findings were consistent over time and from kit to kit.
In what is known as cross validation, the researchers sent the samples to an independent testing lab at the University of Pennsylvania to see if its measurements of the two markers, using the same ELISA tests, were consistent with their own.
“And, for the most part, they were able to validate our data,” Dr. Zaret said.
Focusing on High-Risk, Refining the Test
Their data, Dr. Zaret emphasized, suggest that the two-biomarker test may ultimately be shown to be appropriate for those at high risk of pancreatic cancer, such as individuals who have a first-degree relative who has had the disease or who have certain inherited genetic mutations or a personal history of chronic pancreatitis.
Dr. Srivastava agreed that the test isn’t sufficiently accurate to be used as a screening measure in the general population, where the incidence of pancreatic cancer is only one in every 10,000 people.
An important limitation of the test, Dr. Srivastava said, is that THBS2 is also expressed by other cancer types, although in lower amounts, which may lower the test’s specificity in real-world situations.
“Cancer specificity is an important factor in developing an early detection test,” he explained. If further studies can verify that it’s not highly expressed in other gastrointestinal cancer types, in particular, he added, “that would give encouragement to test this biomarker in the clinic.”
The Penn team is already working on further refining the test. “We’re going to be testing it in larger and larger sample sizes and doing more cross validation,” Dr. Zaret said.
The University of Pennsylvania is setting up a new lab that is separate from Dr. Zaret’s for the additional testing, which will include prospectively collected samples from the Mayo Clinic and the NCI-funded Prostate, Lung, Colorectal, and Ovarian Cancer Screening trial. They’re also planning additional studies and clinical trials of the testing approach in people at high risk for pancreatic cancer.