As the National Cancer Act was passed in 1971, hard-fought and hard-won funding for cancer research began to effect true change. Ground broke, laboratories filled, and our nation's scientific workforce dedicated themselves to a new challenge of transforming how we understand and manage cancer. What we didn't know then is that these investments in the name of cancer would be crucial for our nation to fight future epidemics. The act inadvertently prepared our nation for another deadly illness that was yet to make its ominous appearance.
In 1981, 10 years after the signing of the act, the NIH Clinical Center admitted one of the very first patients with acquired immunodeficiency syndrome (AIDS). He was admitted through an NCI branch that studied immunodeficiency diseases and the cancers afflicting patients with these diseases. Almost immediately after the recognition of AIDS as a new disease, it became apparent that patients with this puzzling syndrome often developed a previously rare cancer called Kaposi sarcoma as well as other tumors such as high-grade B-cell lymphomas. As a result, some of the earliest AIDS patient care and research was performed by NCI scientists and external researchers funded by NCI.
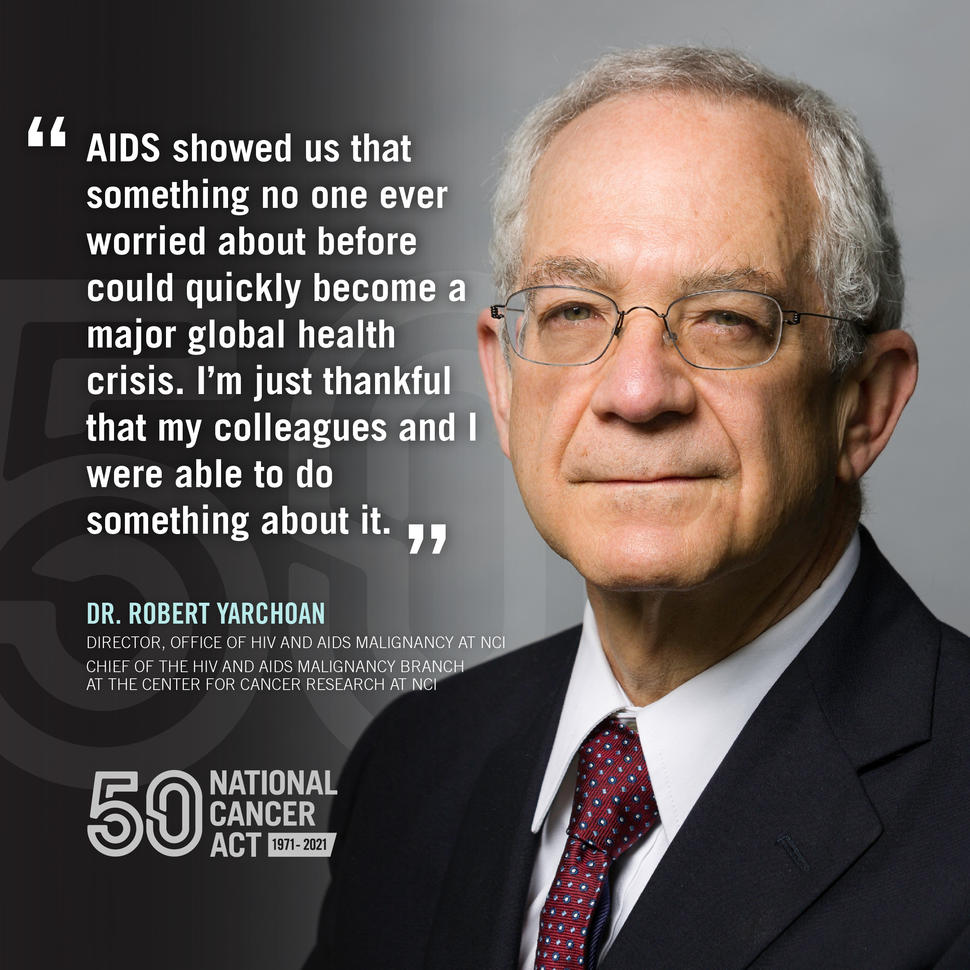
AIDS researcher and early human immunodeficiency virus (HIV) drug developer Robert Yarchoan, M.D., recalled the gravity of the moment: “AIDS showed us that something that no one ever worried about before suddenly could become a major problem for the country and for mankind. And when HIV was identified as the cause of AIDS, it became apparent that in addition to persons known to have AIDS, thousands of people in the United States were already infected with this new virus without knowing it. Moreover, at this time, infection with HIV was in most cases fatal.”
As a result of the investment in cancer research stemming from the National Cancer Act, by the early 1980s NCI was in a strong position to make key early advances in the fight against HIV/AIDS. In particular, NCI and NCI-funded scientists had distinct expertise in retrovirology, in part because of the NCI Special Virus Cancer Program. NCI also had strong programs in immunology and drug development. With these areas of expertise, NCI scientists co-discovered HIV, showed that it was the cause of AIDS, developed the first blood test to prevent the spread of HIV by blood transfusion, and developed the first effective drugs to treat HIV including azidothymidine (also called AZT or zidovudine).
Over the years, NCI developed an extensive portfolio of research in the cancers associated with HIV/AIDS as well as HIV/AIDS itself, and it was recognized that there was a need for a central office to coordinate and prioritize this research. In 2007, NCI, under the leadership of Dr. John Niederhuber, established the Office of HIV and AIDS Malignancy (OHAM) under the Direction of Dr. Yarchoan. The creation of this office was pivotal to NCI. NCI currently funds both intramural (within NCI buildings) and extramural (through grants and contracts) research in HIV/AIDS and HIV-associated malignancies. In addition to coordinating HIV/AIDS and HIV- malignancy research throughout NCI, OHAM directly manages and facilitates major programs and initiatives through research, training, international studies, and clinical trials. As the needs and opportunities for research change, NCI’s OHAM plays a crucial role in prioritizing the most important research to prevent, diagnose, and treat HIV-associated malignancies and other cancers in people living with HIV, as well as basic research on these cancers and HIV/AIDS itself.
“Coordinating HIV/AIDS research throughout NCI, with the NIH Office of AIDS Research, and with other institutes and centers is a challenging task. However, doing it well enables us to make sure that funds are directed into the areas where they are most needed,” said RaeJean Hermansen, Ph.D., special assistant to the director of OHAM.
Two of the main efforts overseen by OHAM are the AIDS Malignancy Consortium, which conducts clinical research in HIV-associated malignancies both in the United States and in resource-poor areas, including sub-Saharan Africa, and the AIDS and Cancer Specimen Resource, which helps researchers by coordinating tissue donations from patients with HIV/AIDS. “It is very gratifying to have contributed to managing vital programs that focus on improving the standard of care of people living with HIV and cancer and ease their sufferings,” said Mostafa Nokta, M.D., Ph.D., director, AIDS Cancer Clinical Program, OHAM, NCI.
One of the challenges of OHAM is to adjust research priorities as needs and opportunities change. “With the development of antiretroviral therapy, we initially saw a dramatic decrease in AIDS-defining cancers. However, as people living with HIV are surviving and aging, we are seeing an increase in other cancers, and cancer continues to be a significant morbidity and one of the most frequent causes of death,” said Geraldina Dominguez, Ph.D., director, AIDS Malignancy Program, OHAM.
The National Cancer Act paved the way for the resources, skills, and expertise to be in place for those at the forefront of HIV/AIDS research. It enabled major advances in a time of need and NCI looks forward to robust cross-fertilization between cancer research and HIV/AIDS research until we have addressed every challenge that comes our way.
Although many doubted whether any drug could be developed to fight AIDS, Dr. Robert Yarchoan worked with Drs. Samuel Broder and Hiroaki Mitsuya on the first AIDS drugs, including azidothymidine (AZT), transforming a fatal disease into a chronic one.