Simple Hysterectomy May Expand Treatment Options for Early-Stage Cervical Cancer
, by Edward Winstead
Most people with early-stage cervical cancer are treated with a radical hysterectomy. But doctors have long wondered whether a less extensive surgery could be a safe and effective alternative to the radical procedure.
According to the results of a large clinical trial, the answer seems to be yes. In the trial, 700 people with early-stage cervical cancer underwent either a radical hysterectomy or a more limited surgical procedure called a simple hysterectomy.
Three years after surgery, the cancer had come back in the pelvic area among less than 3% of the participants, regardless of which procedure they had undergone, researchers reported in the New England Journal of Medicine on February 29.
However, participants who had a simple hysterectomy experienced fewer side effects, such as urinary incontinence and urinary retention (trouble emptying all of the urine from the bladder), than those who had a radical hysterectomy. Measures of quality of life appeared to favor the simple over the radical hysterectomy, the researchers found.
“Both surgeries have similarly low rates of cancer recurrence,” said study leader Marie Plante, M.D., of Université Laval in Quebec. “But the less radical surgery was associated with fewer surgical complications and a better quality of life.”
The study was a noninferiority trial, meaning it was not designed to determine which procedure was better, Dr. Plante noted; rather, the goal was to determine whether a simple hysterectomy was not worse than the radical procedure for preventing a recurrence.
Pedro Ramirez, M.D., of Houston Methodist Hospital, who wrote an accompanying editorial, predicted that a simple hysterectomy will likely become the new standard treatment for people with early-stage, low-risk cervical cancer as defined in the trial.
The research, Dr. Ramirez explained, is part of an effort by cancer surgeons to de-escalate treatment, by shifting away from radical procedures toward more conservative approaches that may have fewer side effects.
“This trial so far shows that by de-escalating the treatment, we are not compromising outcomes for patients,” Dr. Ramirez said.
Complications, side effects, and limitations of the trial
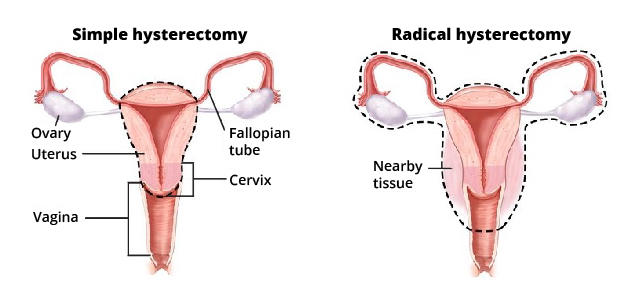
During a simple hysterectomy, a surgeon removes the uterus and the cervix. By comparison, a radical hysterectomy involves removing the uterus, cervix, part of the vagina, and ligaments and tissues around the uterus (parametrium).
The radical surgery has long been the recommended treatment for people diagnosed with early-stage cervical cancers considered to be at low risk of the cancer spreading or coming back. Studies have suggested that only about 1% of low-risk, early-stage cervical cancers spread to the tissue near the cervix.
“We have wondered whether it’s necessary to do such a radical surgery for a cancer with such a low probability of spread to the surrounding tissues,” said Dr. Plante. Such questions were the basis for developing the SHAPE trial.
The Canadian Cancer Trials Group led the study, which was funded by the Canadian Institutes of Health Research and Canadian Cancer Society, in collaboration with the Gynecologic Cancer Intergroup.
Almost identical recurrence rates with simple hysterectomy
All participants in the trial had early-stage cervical cancer that met certain low-risk criteria (see box). All participants had surgery to remove lymph nodes in the pelvis (lymph node dissection) and then were randomly assigned to get a simple or radical hysterectomy.
With a median follow-up of 4.5 years, the 3-year pelvic recurrence rate was 2.52% in the simple hysterectomy group and 2.17% in the radical hysterectomy group.
There were more surgical complications in the radical hysterectomy group. Those participants had three times as many bladder injuries and nearly twice as many ureteral complications as participants who had a simple hysterectomy.
In addition, urinary incontinence was more common in the radical hysterectomy group (5.5% versus 2.4% within 4 weeks of surgery) and persisted over time (11% versus 4.7% beyond 4 weeks), the researchers found.
Urinary retention was also higher in the radical hysterectomy group (11% versus 0.6% within 4 weeks of surgery) and persisted over time (9.9% versus 0.6% beyond 4 weeks).
The researchers also assessed participants’ quality of life using questionnaires. People in the simple hysterectomy group had much more favorable responses to questions about topics such as sexual function, pain, and distress.
After extended follow-up, Dr. Plante and her colleagues plan to publish additional results related to quality of life. They also intend to analyze the relative costs of the two surgical procedures.
The researchers noted some limitations of the trial. Participants were primarily from Western Europe, South Korea, and Canada. Black women and Native Americans were underrepresented in the trial, and consequently the findings may not apply to these groups or to populations in developing nations, they wrote.
They also cautioned that the results could change with longer follow-up, though most recurrences occur within the first 2 years after surgery.
Patient selection for the simple hysterectomy is key
Dr. Plante stressed the need to carefully select patients for the simple hysterectomy.
“We have to ensure that their tumors meet the criteria established during this trial,” she said.
Dr. Ramirez agreed. He noted that half of the hysterectomies were done by laparoscopy (also called minimally invasive surgery), and those were split almost evenly between robotic procedures and traditional laparoscopic surgery.
“The SHAPE trial was not designed to determine whether one type of surgery for simple hysterectomy is better than another,” Dr. Ramirez said.
Nonetheless, the trial results will be “impactful for our patients,” he said.
“This research is a very positive step forward for people diagnosed with cervical cancer.”