What is constipation?
Constipation is the slow movement of stool (poop) through the large intestine. The longer it takes for the stool to move through the large intestine, the more it loses fluid and the drier and harder it becomes.
If you are constipated, you may be unable to have a bowel movement, need to push harder to have a bowel movement, or have fewer than your usual number of bowel movements. Talk to your doctor if you have constipation. Your doctor can recommend medicines and other ways for treating constipation caused by cancer and cancer treatment.
Constipation may last for a short time, or it may be chronic and last for a long time. Long-term (chronic) constipation can lead to fecal impaction or bowel obstruction, two potentially life-threatening conditions that require immediate medical care. Learn more at What is fecal impaction? and Bowel Obstruction.
What are signs and symptoms of constipation?
Learn about other digestive system problems in people with cancer
Signs and symptoms of constipation include:
- having two or fewer bowel movements in one week
- dry, hard, or lumpy stool
- pain during a bowel movement
- difficulty having a bowel movement
- stomach pain or cramps
- feeling bloated or nauseous
What causes constipation in people with cancer?
Constipation in people with cancer may be caused by:
- Certain types of cancer. Constipation may be a sign or symptom of cancers that push on organs in the abdomen, block the movement of stool through the bowel, or affect the nerves in your spine connected to your bowel. Some cancers that may cause constipation include colon cancer, rectal cancer, ovarian cancer, and brain tumors.
- Cancer treatments such as chemotherapy. Constipation is a common side effect of some types of chemotherapy.
- Medicines. Many medicines, including opioid pain medications, antianxiety drugs, antinausea drugs (antiemetics), and diuretics, can cause constipation.
- Lifestyle and dietary changes. When you are getting cancer treatment, you may have less energy for exercise and your appetite and diet may change. Being less active and eating different foods than normal can cause constipation.
How is constipation diagnosed in people with cancer?
Finding the cause of constipation is important so you can get relief and avoid serious problems such as fecal impaction. Your doctor will do a physical exam, which will include looking at and feeling the abdomen for areas of swelling or firmness and listening to the sounds of your bowels. Your doctor may also ask questions such as:
- How often do you have a bowel movement? How often did you have a bowel movement before you had cancer? Has there been a recent change in your bowel habits?
- When was your last bowel movement? What was it like (how much, hard or soft, what color, was there blood)? Did you have to push more than usual?
- Do you have a fever, cramps, a feeling of fullness near the rectum, pain, or bloating?
Your doctor may be able to diagnose constipation and suggest treatment based on a physical exam and these questions. Sometimes, your doctor may need to do other tests to better understand what is causing constipation:
- Digital rectal examination (DRE): A physical exam in which the doctor or nurse inserts a lubricated, gloved finger into the lower part of the rectum to feel for impacted stool or unusual changes.
- X-rays: An x-ray is a type of radiation that, in low doses, can be used to make a picture of areas inside the body. An x-ray of the abdomen can show a tumor or fecal impaction that may be causing constipation.
Ways to prevent and treat constipation
If your doctor thinks your cancer or cancer treatments will cause constipation, they will give you tips and prescribe medicine to prevent it. If you become constipated, your doctor will recommend many of these same tips and medicines to help you get relief. Talk with your health care team about what treatment is right for you.
Tips for managing constipation
- Drink plenty of liquids. Drinking 8 cups of water or clear liquids per day can help you stay hydrated, which helps with constipation. Beverages such as coffee and prune juice can have a laxative effect, and hot drinks can also help stool move through the bowel.
- Try to be active every day. Ask your health care team about exercises you can do. Walking, riding a bike, and practicing yoga may be options for you. You can also do light exercise in a bed or chair.
- Eat at the same time each day. This routine can help you get back to your normal number of bowel movements.
- Keep a record of your bowel movements. Showing this record to your health care team and talking to them about what is normal for you can help your doctor treat the constipation you are experiencing.
- Talk with your doctor about dietary fiber. High-fiber foods and fiber supplements can make constipation worse for some people. Ask your doctor if adding fiber to your diet will help relieve constipation for you.
What can people with cancer take for constipation?
Your doctor may prescribe medicines called laxatives that help prevent or relieve constipation. Use only medicines and treatments for constipation that your doctor recommends. Many different types of laxatives are available, and your doctor may recommend others not listed here:
- Osmotics pull water into the bowel from other parts of the body, making it easier to have a bowel movement. Polyethylene glycol (MiraLAX), magnesium hydroxide (Milk of Magnesia), lactulose (Enulose), and sorbitol are examples of osmotic laxatives.
- Stool softeners, or emollients, soften poop by increasing the amount of water and fat that the poop absorbs. Docusate (Colace) is an example of a stool softener.
- Stimulant laxatives cause the intestines to contract so stool moves through the bowel. Bisacodyl (Correctol), senna (Senokot), and castor oil are examples of stimulant laxatives.
Do not use suppositories (capsules you insert into your anus) or enemas (liquid medicine that you inject into your anus) unless your doctor recommends them. In some people with cancer, these treatments may lead to bleeding, infection, or other harmful side effects.
How a caregiver can help
- Encourage the person you are caring for to drink plenty of water or other fluids. Make sure they also have access to hot beverages and prune juice, which may help relieve constipation.
- Help the person you are caring for stay physically active. Physical activity includes moving from a bed to a chair, walking short distances, or riding an exercise bike. Talk to their care team to find out what exercise is right for them.
- Monitor the person’s bowel movements and help them keep a record of their bowel movements. They should have a bowel movement every day or every other day that is not hard and does not require straining.
- Notify the care team if the person has had fewer than three bowel movements in one week or is experiencing severe abdominal pain, vomiting, and other signs of fecal impaction.
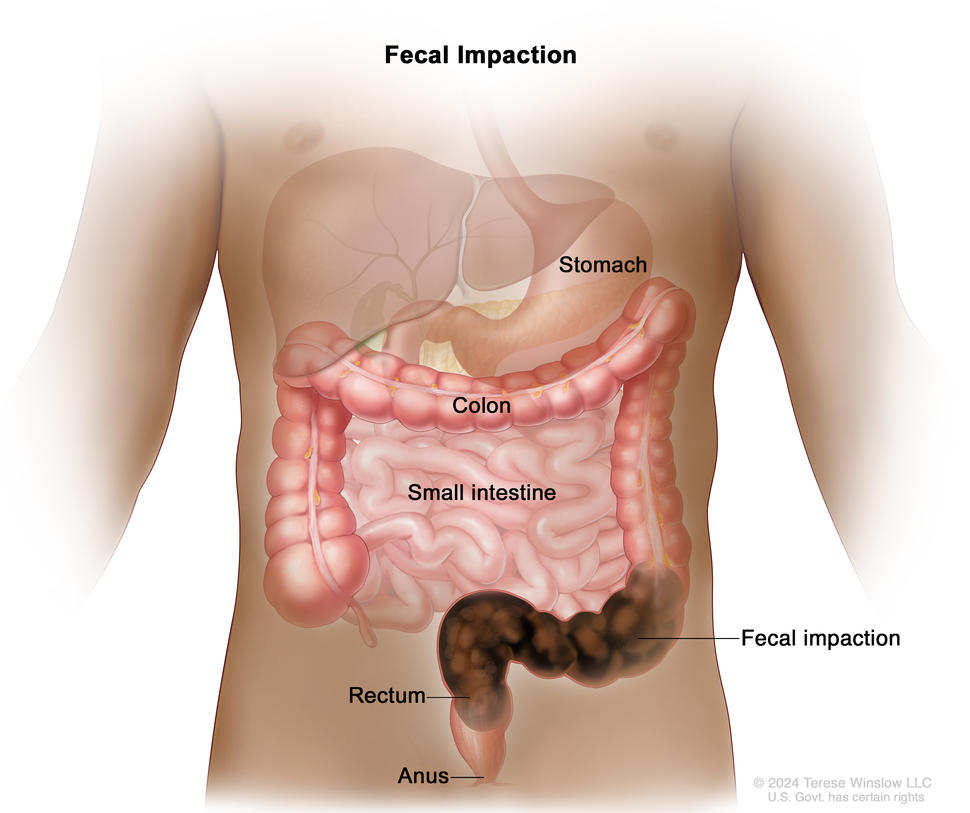
What is fecal impaction?
Fecal impaction is a serious condition in which hardened stool blocks the colon or rectum. Unlike constipation, fecal impaction can be life-threatening and requires immediate medical attention.
What causes fecal impaction?
Causes of fecal impaction include:
- opioid pain medicines
- little or no physical activity over a long period
- dietary changes
- constipation that is not treated
- inability to push stool out because of weakness or muscle problems
What are signs and symptoms of fecal impaction?
Signs and symptoms of fecal impaction include:
- chronic constipation
- a feeling of pressure in the rectum or incomplete emptying of stool
- lower back pain or pain in the abdomen
- urinating more or less often than usual or being unable to urinate
- breathing problems, rapid heartbeat, confusion, dizziness, low blood pressure, and bloating
- sudden, explosive diarrhea or leaking stool (as stool moves around the impaction)
- nausea and vomiting
- dehydration
How is fecal impaction diagnosed in people with cancer?
Fecal impaction is diagnosed in the same way as constipation. To learn more, go to How is constipation diagnosed in people with cancer?
How is fecal impaction treated?
The main treatment for fecal impaction is to moisten and soften the stool using an enema. The softened stool can then pass out of the body. Because enemas can be dangerous for people with cancer, they should be used only when prescribed and given by a doctor.
You may need to have stool manually removed from the rectum after it is softened. Laxatives are generally not used to treat fecal impaction because they may cause cramping and damage to your intestines.
Talking with your doctor about constipation
Tell your doctor or nurse if you are having constipation so you can get treatment as soon as possible. Treating constipation early can help prevent serious problems like fecal impaction and bowel obstruction. Your doctor can help you find ways to treat and manage this side effect of cancer and cancer treatment.
Questions to ask your provider about constipation:
- What symptoms or problems should I call you about?
- Should I take medicine for constipation? If so, what medicine should I take? What medicine should I avoid?
- How much liquid should I drink each day?
- What foods can help with constipation? What foods should I avoid?
- Could I meet with a registered dietitian to learn more?
Getting support if you have constipation
Side effects like constipation or fecal impaction can be hard to deal with, both physically and emotionally. It’s important to ask for support from your health care team. They can help you prepare for and make it through difficult times. Learn more about ways to cope with cancer, including ways to adjust to daily life during cancer treatment.
For family members and friends who are caring for someone with cancer, you may find these suggestions for caregivers to be helpful.