NCI researchers develop approach that could help supercharge T-cell therapies against solid tumors
- Posted:
240-760-6600
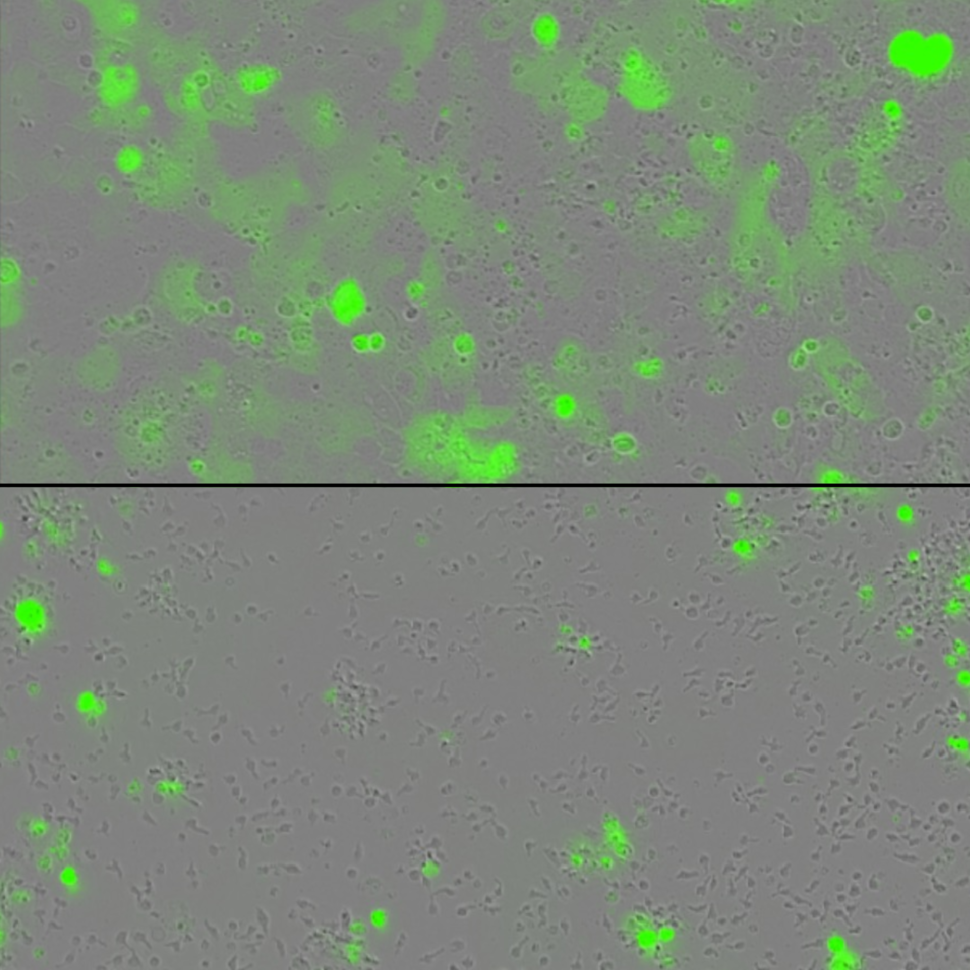
Tumor cells (green) are grown in a dish with engineered T cells alone (on the top) or with engineered T cells harboring two cytokines tethered to the surface (bottom image) . The engineered T cells containing the tethered cytokines lead to greater eradication of tumors.
Credit: Credit: Rosa Nguyen, National Cancer Institute
What
Researchers at the National Cancer Institute (NCI), part of the National Institutes of Health, have developed a way to potentially increase the effectiveness of T cell–based immunotherapy treatments, such as CAR T-cell therapy, against solid tumors. T cells are specialized white blood cells of the immune system that eliminate infected or abnormal cells. In animal studies, the enhanced T-cell therapies were effective against cervical cancer and neuroblastoma, a common solid tumor in children. The findings appear Nov. 1, 2023, in Clinical Cancer Research.
CAR T-cell therapy is a form of cellular immunotherapy that involves engineering T cells in the laboratory so they can specifically target and kill tumors. CAR T-cell therapy has been successful in treating blood cancers, but it hasn’t worked well for solid tumors. To improve the effectiveness of T-cell therapy against solid tumors, researchers at NCI’s Center for Cancer Research engineered T cells (CAR T cells and another form of cellular immunotherapy called TCR T cells) to carry cytokines, which are proteins that can boost T-cell function.
In laboratory studies, CAR and TCR T cells modified to express the cytokines IL-15 and IL-21 on their surface killed far more cancer cells than T cells carrying just one of these cytokines or neither of them. Previous research has found that treating patients with large amounts of cytokines caused severe, potentially fatal, side effects. The new approach aims to deliver this cytokine boost in a much more targeted way.
In a mouse model of cervical cancer, T cells carrying both cytokines shrank tumors completely in 4 of 5 mice, compared with just 1 of 5 mice treated with T cells carrying a single cytokine. Mice treated with T cells carrying both cytokines also lived longer than mice treated with T cells carrying just one cytokine. The approach also showed potential in mouse models of pediatric neuroblastoma, a difficult-to-treat form of childhood cancer for which new therapies are desperately needed. In these models, treatment with T cells carrying both cytokines shrank tumors to a greater extent than treatment with T cells carrying one or no cytokines. In the cervical cancer and neuroblastoma models, T cells carrying the cytokine pair did not cause any serious side effects.
The researchers are continuing to test the IL-15- and IL-21-expressing T-cell therapies in lab and animal model studies of other solid tumors, with the goal of translating the approach into human clinical trials in the next few years.
Who
Rosa Nguyen, M.D., Ph.D., Center for Cancer Research, National Cancer Institute
About the National Cancer Institute (NCI): NCI leads the National Cancer Program and NIH’s efforts to dramatically reduce the prevalence of cancer and improve the lives of people with cancer. NCI supports a wide range of cancer research and training extramurally through grants and contracts. NCI’s intramural research program conducts innovative, transdisciplinary basic, translational, clinical, and epidemiological research on the causes of cancer, avenues for prevention, risk prediction, early detection, and treatment, including research at the NIH Clinical Center—the world’s largest research hospital. Learn more about the intramural research done in NCI’s Center for Cancer Research. For more information about cancer, please visit the NCI website at cancer.gov or call NCI’s contact center at 1-800-4-CANCER (1-800-422-6237).
About the National Institutes of Health (NIH): NIH, the nation's medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit nih.gov.